2026 GOLD Report Updates
Discover what’s new in the 2026 GOLD COPD Report including earlier detection, new risk definitions, treatment updates, and emerging tech shaping patient care.

Every year, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) releases a new report on the diagnosis, assessment, prevention, and management of Chronic Obstructive Pulmonary Disease (COPD). The GOLD Report is put together by an international team of experts on the topic and is considered the gold standard (no pun intended) for COPD care across the globe. This year is no different, with the 2026 GOLD Report recently being released in November 2025. The 2026 report includes some important new guidance that clinicians need to know.
Emphasis on Early Diagnosis
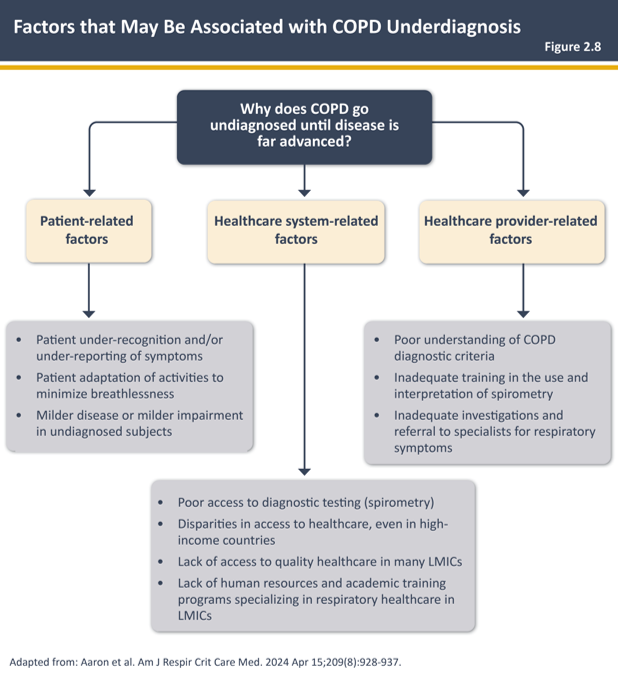
Underdiagnosis is one of the most prevalent and harmful problems in COPD care. Underdiagnosis refers to people who have COPD but have not been formally diagnosed. This is actually extremely common, as it is estimated that 70-80% of COPD cases worldwide remain undiagnosed. This can be due to a variety of factors, such as underuse of spirometry, symptom misinterpretation, and overlap with other health conditions. Timely diagnosis can meaningfully impact long-term patient outcomes by getting patients on an appropriate treatment plan and preventing physically damaging exacerbations and financially damaging hospitalizations. The 2026 report recognizes the importance of identifying at-risk individuals sooner, particularly those with smoking or environmental exposures who present with subtle or intermittent symptoms. Refined screening figures on who should receive spirometry, updated risk factor profiles, and new algorithms are ways to target at-risk patients and diagnose COPD sooner, leading to earlier treatment and better outcomes for patients.
--> A diagnosis of COPD should be considered in any patient who has dyspnea, chronic cough or sputum production, a history of recurrent lower respiratory tract infections and/or a history of exposure to risk factors; spirometry with post-bronchodilator FEV1/FVC <0.7 is mandatory to establish the diagnosis of COPD
--> Pre-bronchodilator spirometry can be used to exclude a diagnosis of COPD
- Tobacco smoke
- Inhalation of toxic particles and gases from household or outdoor air pollution
- Genetic factors (epidemiologically rare)
Change in Exacerbation Guidance
The new report introduced a major shift in the definition of exacerbation risk. Now, just one moderate or severe exacerbation in the previous year is considered a marker of increased clinical risk. Previously, patients were considered low risk unless they experienced 2 or more moderate exacerbations or 1 or more severe exacerbations. This shift is supported by evidence that any exacerbation can accelerate a decline in the patient's lung function. This new guidance encourages clinicians to reassess a patient’s treatment efficacy promptly instead of waiting for a pattern to form. GOLD emphasizes the need for rapid assessment, prompt pharmacologic intervention, and thoughtful post-exacerbation evaluation. This approach includes verifying inhaler technique, assessing medication adherence, reviewing comorbidities, and ensuring that medication therapy is optimized. Pivoting our viewpoint of exacerbations from isolated incidents to warning signs promotes earlier intervention and more proactive disease management, both of which are recurring themes in this new report.
Disease Activity
A new concept introduced in the 2026 report is “disease activity.” COPD severity is traditionally determined largely by FEV₁ measurements and symptom scores, but these metrics often fail to capture how quickly a patient’s condition is evolving. The new focus on activity encourages clinicians to consider the trajectory of the disease rather than focusing on its current state. A patient with stable lung function over two years may require very different management than someone whose symptoms are rapidly worsening or who has experienced frequent exacerbations. By shifting attention toward the trajectory of the disease, clinicians can implement a more personalized treatment approach and change the course of the disease before it is too late.
New Treatment Framework
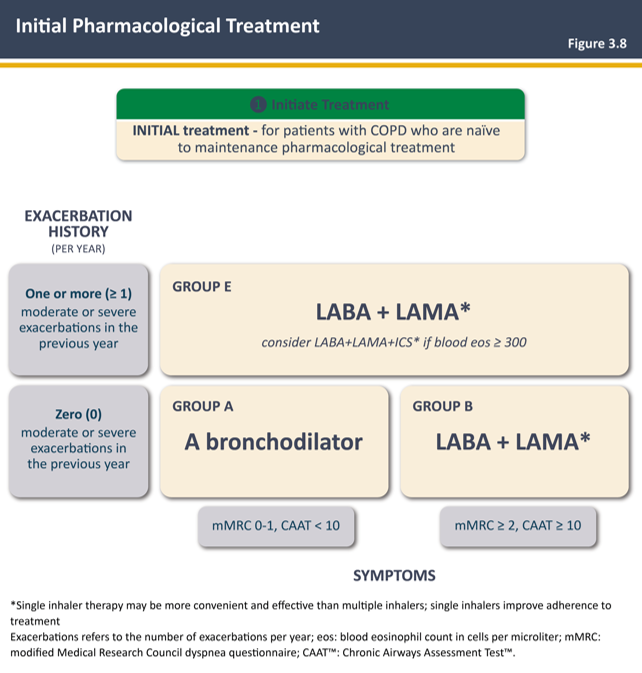
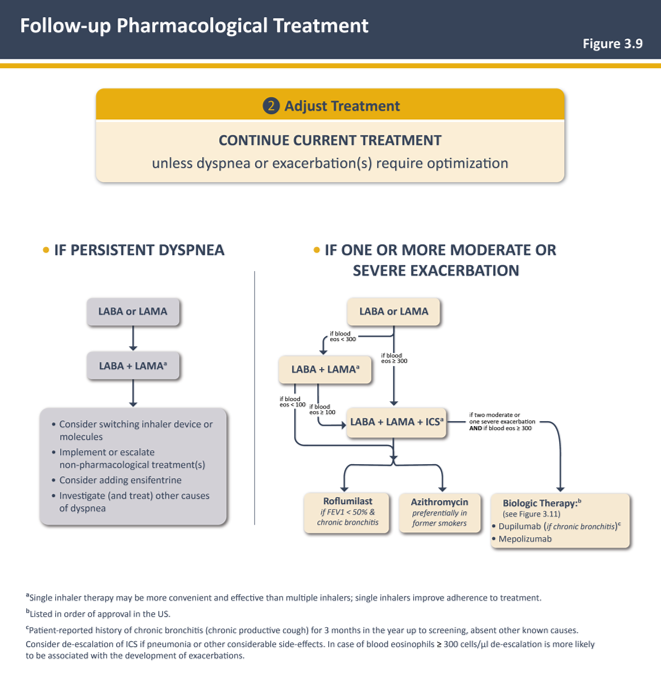
The pharmacologic treatment section has been reorganized to better differentiate guidance between patients who are new to treatment and those who are already receiving maintenance therapy. A treatment algorithm is provided for both scenarios. This clearer separation makes the recommendations easier to apply in real-world situations. For new patients, GOLD reinforces long-acting bronchodilators (LABAs) as the foundation of therapy, but also includes clearer guidance on when to begin with single bronchodilator therapy instead of dual bronchodilator therapy. For those already on maintenance treatment, the updated framework encourages clinicians to reassess whether current therapy is truly effective before escalating. This includes checking inhaler technique, adherence, device suitability, and any comorbid conditions that may be affecting symptoms. The report also refreshes its recommendations on vaccinations and emphasizes that preventive measures and lifestyle modification remain key components of COPD management.
Emerging Technology
One of the newest additions to the 2026 report is a chapter dedicated to emerging technologies and artificial intelligence. While these tools are not meant to replace clinical judgment, they show promise in improving and streamlining how COPD is monitored and managed. Digital inhalers that track usage, remote monitoring programs that pick up early signs of worsening symptoms, and AI risk prediction models are becoming more common in both research and clinical practice. GOLD doesn’t make any sweeping recommendations about adopting these tools, but it recognizes that they can help clinicians identify disease activity earlier and support patients who struggle with symptom awareness or consistent inhaler use.
What This Means for Clinicians
Overall, the 2026 GOLD Report encourages a shift toward earlier recognition, closer follow-up, and more individualized treatment. For clinicians, this means taking even subtle symptoms seriously, reevaluating treatment after a single exacerbation, and checking in on inhaler technique and medication adherence (both of which are great opportunities for pharmacists to be involved). The updated guidance represents a shift from reactive treatment to proactive treatment, with an emphasis on catching problems before they escalate. These changes can help prevent avoidable exacerbations, maintain lung function longer, and improve quality of life for COPD patients.
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2026 report. Accessed November 30, 2025. https://goldcopd.org/2026-gold-report-and-pocket-guide/
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.

