Always Check the Thyroid
An often overlooked organ, the thyroid can effect numerous metabolic processes and development pathways in the human body if not functioning properly. In this week's article, we are going to discuss the importance of checking the thyroid, and what to do when there is dysfunction present.

Your patient presents with fatigue, consistent complaints of being cold, weight gain over the past few months, and has been feeling "down" about life recently. All the blood work, vital signs, and imaging returns normal. There is no obvious disease or lab value to blame for their symptoms. What could possibly be wrong?
You look at your attending/preceptor with confusion. All they say in return are six simple words: "Well, did you check the thyroid?"
An often overlooked organ, the thyroid can effect numerous metabolic processes and development pathways in the human body if not functioning properly. In this week's article, we are going to discuss the importance of checking the thyroid, and what to do when dysfunction is present.
Disclaimer: This post is meant to provide an overview of a clinical topic that may include (but is not limited to) information on pathophysiology, diagnosis, treatment, clinical pharmacology, medication management, adverse effects, and clinical pearls. References are included at the bottom of each post. This post is not to be used as medical advice for direct patient care, but as a guide for learning and discussion.

Introduction
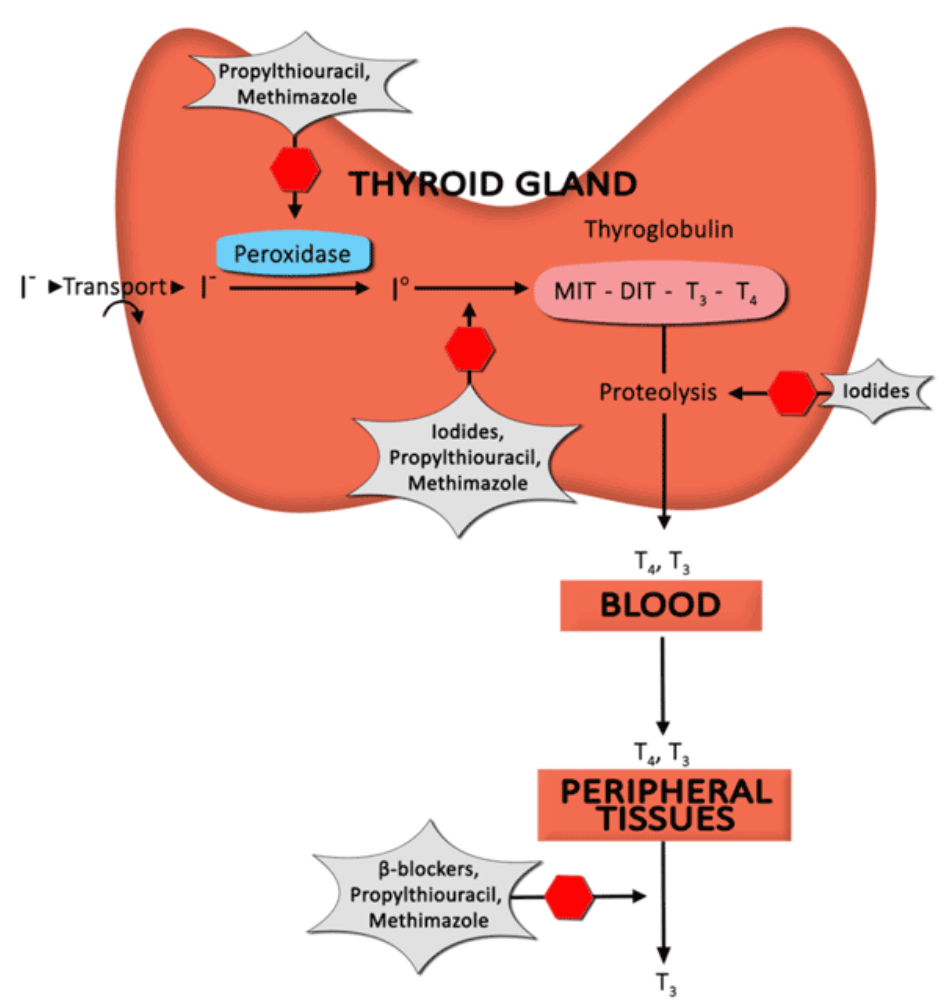
Your thyroid is a butterfly-shaped gland in your neck that secretes hormones: triiodothyronine (T3) and thyroxine (T4). T4 is converted to T3 by peripheral tissues. T4 and T3 circulate throughout the body by binding to proteins in the blood (albumin, thyroxine-binding globulin, and trans-thyretin). Only the T3 that is unbound (free) is biologically active. It is important to note that thyroid hormones contain iodine. This will be discussed with pharmacotherapy options later in the article.
The thyroid gland does not constantly release T4 and T3, however. The thyroid gland is regulated by the pituitary gland, which in turn is regulated by the hypothalamus. This is known as the hypothalamus-pituitary-thyroid axis (see figure below).
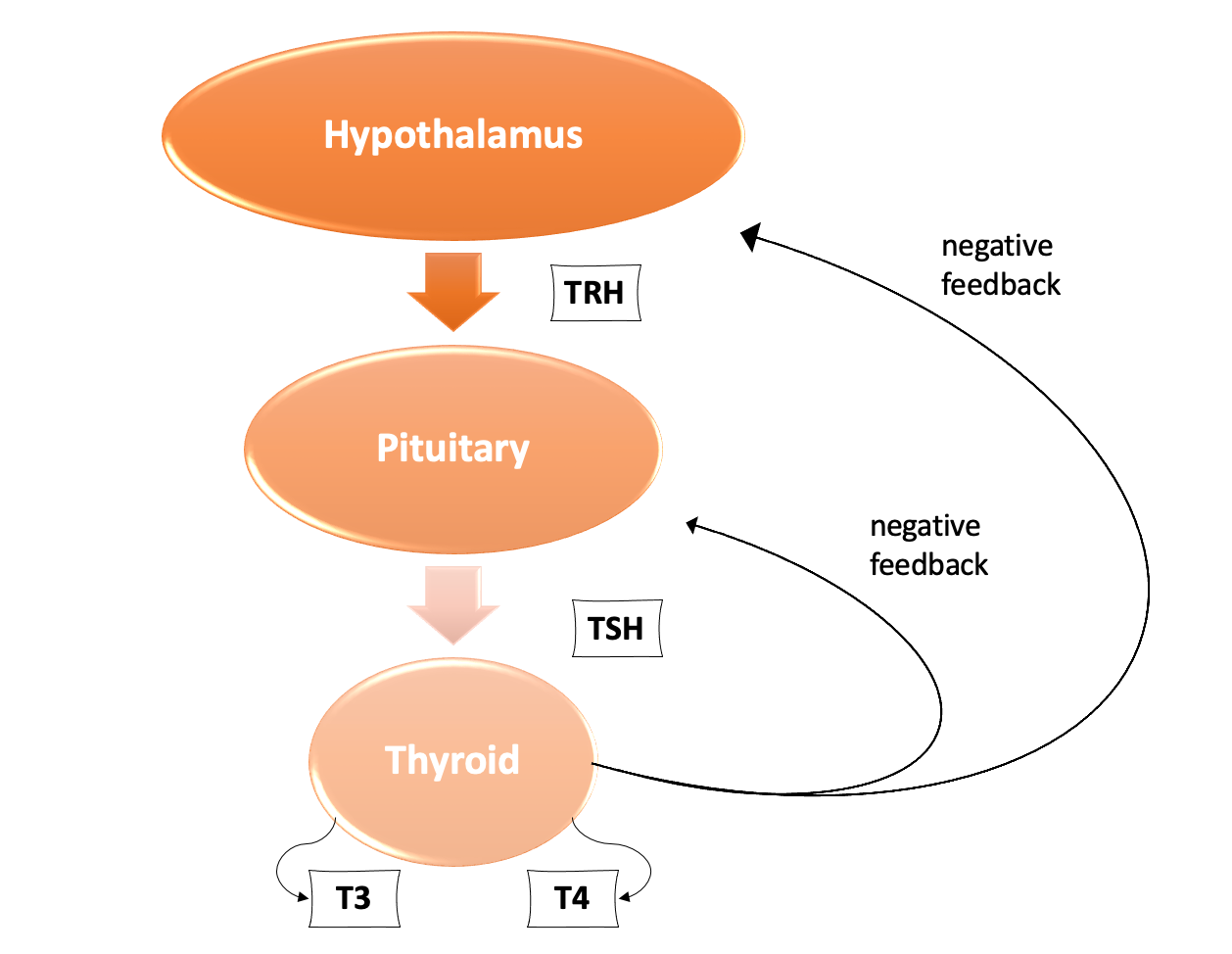
The hypothalamus will release thyroid releasing hormone (TRH) which will stimulate the pituitary gland to release thyroid stimulating hormone (TSH). TSH acts on the thyroid gland to release T4 and T3. T4 and T3 have negative feedback on both the pituitary gland and hypothalamus. This keeps the axis in homeostasis (balance). When T4 and T3 are low, TRH and TSH are released. When T4 and T3 concentrations are high, TRH and TSH are suppressed.
The thyroid hormones are important for growth and development. When the body cannot regulate the hypothalamus-pituitary-thyroid axis, and homeostasis is lost, clinical hyper- or hypo- thyroidism can arise. We will discuss both of these in more detail below!
Normal lab values to note prior to our discussion:
- T4: 0.9 - 2.3 ng/dL
- T3: 60 - 180 ng/dL
- TSH: 0.5 - 5.0 mIU/L
Hyperthyroidism
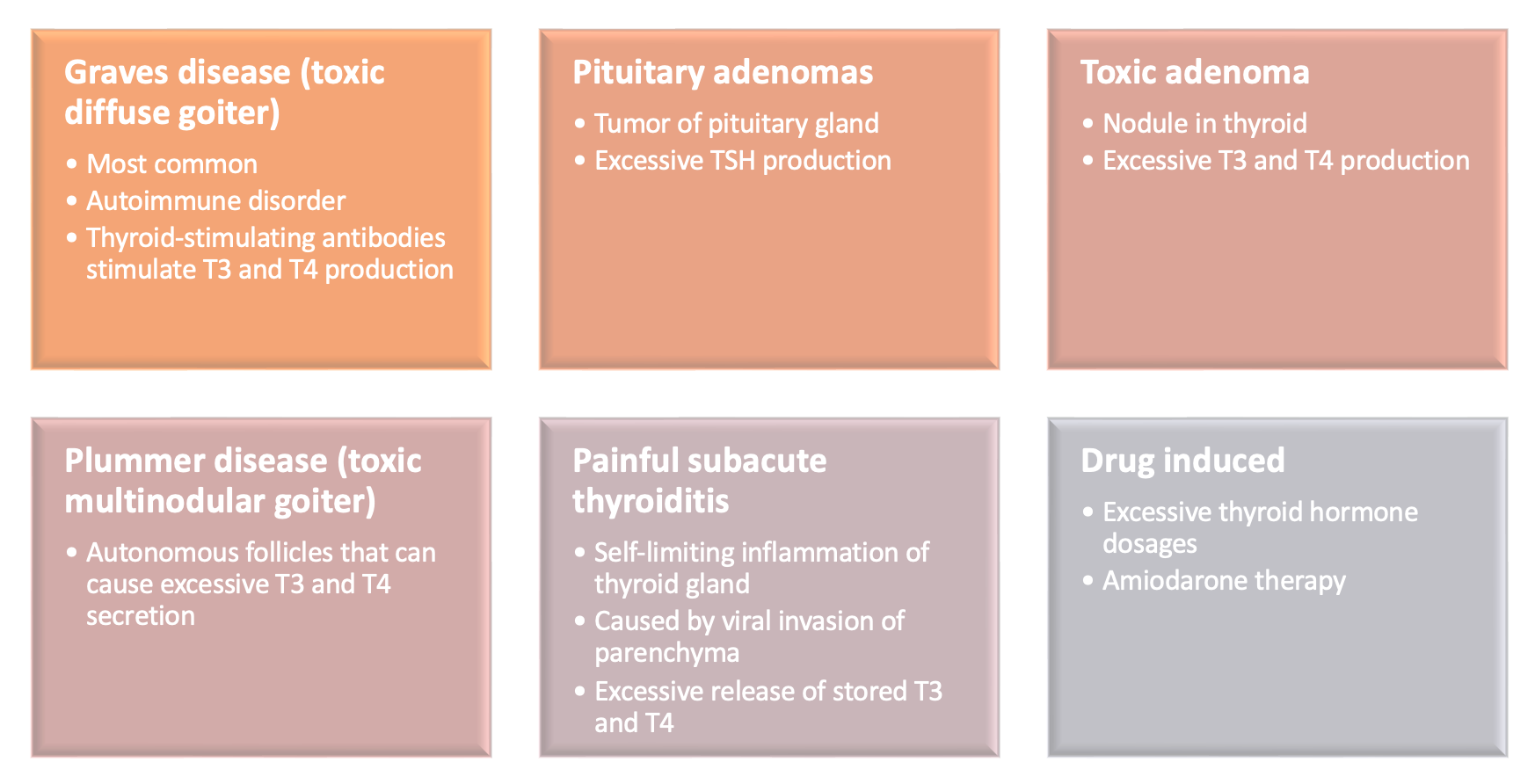
The first step when navigating HYPERthyroidism is understanding why the patient has elevated T4 and T3 levels. There are a variety of mechanisms:
Diagnosis
Laboratory values indicative for hyperthyroidism include:
- Elevated T4
- Suppressed TSH (except in TSH-secreting adenomas)
- Possible presence of thyroid-related antibodies
Presentation
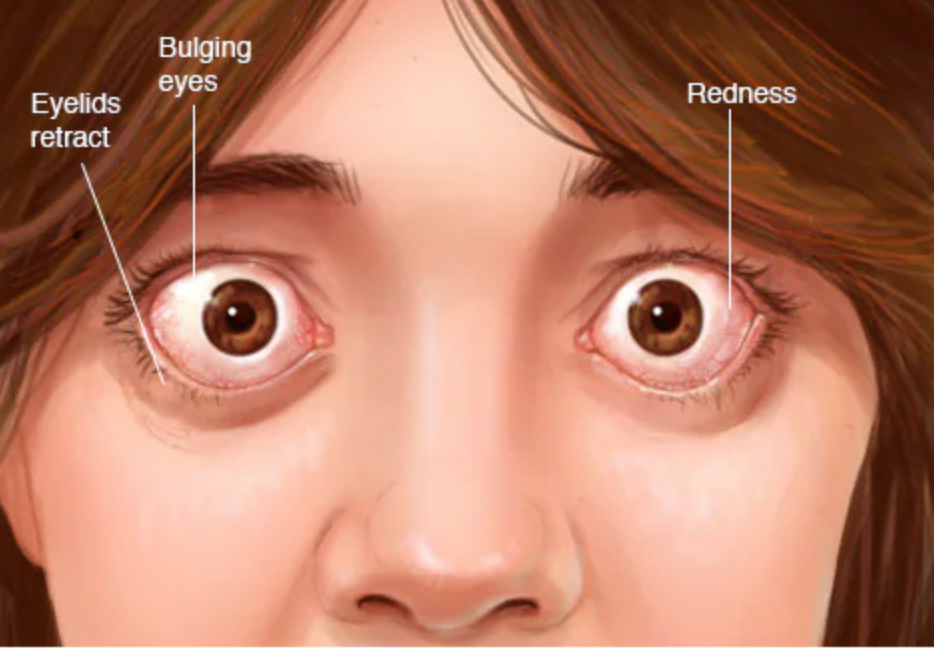
Variety of symptoms from over stimulation and growth (not an all-inclusive list): weight loss, heat intolerance, goiter, fine hair, heart palpitations, anxiety, insomnia, menstrual disturbances, sweating, warm skin, exophthalmos
Treatment
1. Ablative therapy (results in HYPOthyroidism)
2. Thyroidectomy (surgery to remove the thyroid gland all together – this leaves the patient chronically HYPOthyroid)
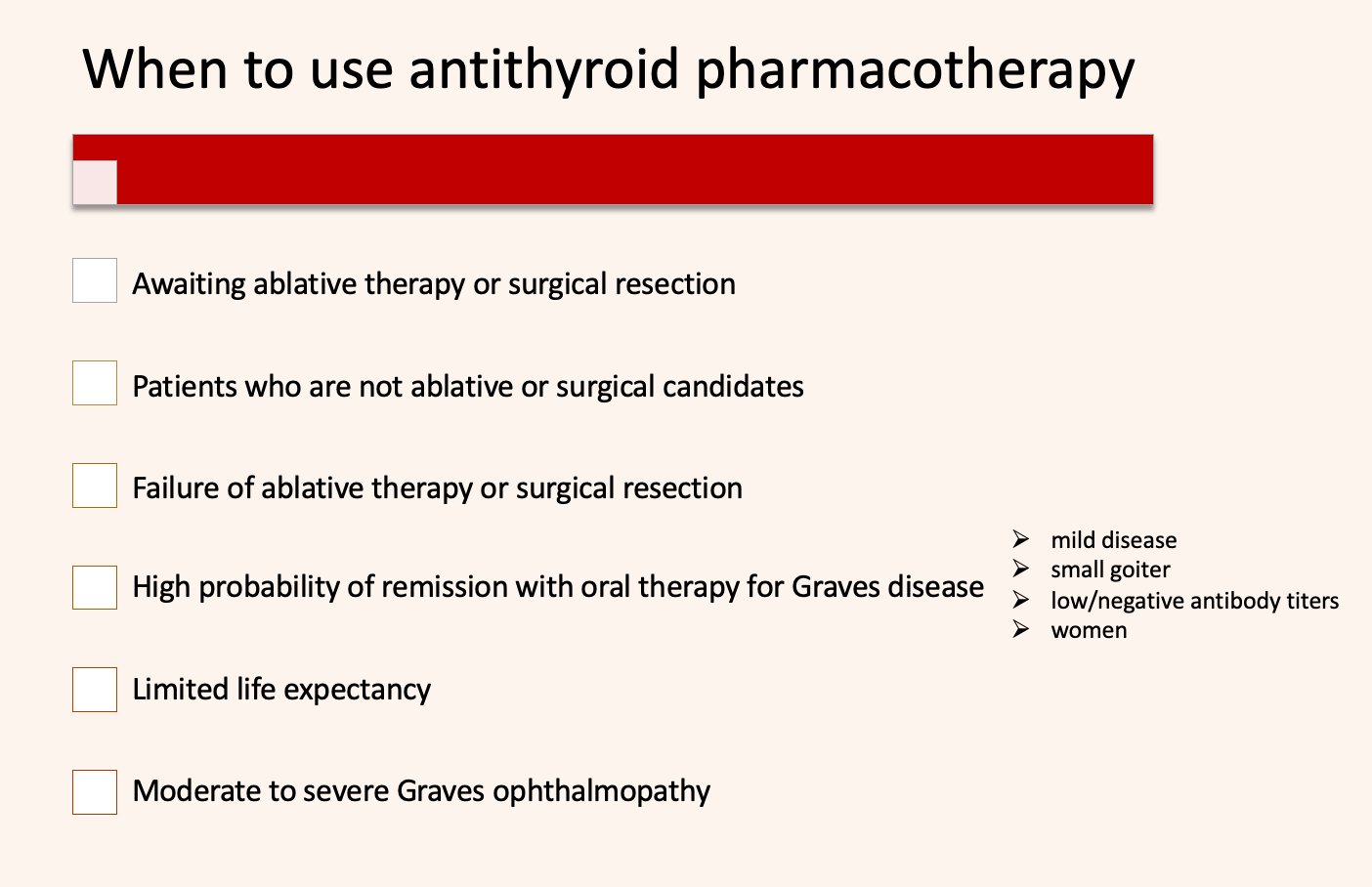
3. Pharmacotherapy (bullets 3a-3c)
3a. Thioureas
- Mechanism: inhibit iodination and synthesis of thyroid hormones
- Propylthiouracil (PTU): given 2-3 times daily, recommended in first trimester of pregnancy due to risk of embryopathy with methimazole
- Methimazole (MMI): given daily; the preferred agent for Graves disease; can be used in the second and third trimester of pregnancy
- Maximal effect may take 4-6 months for both medications
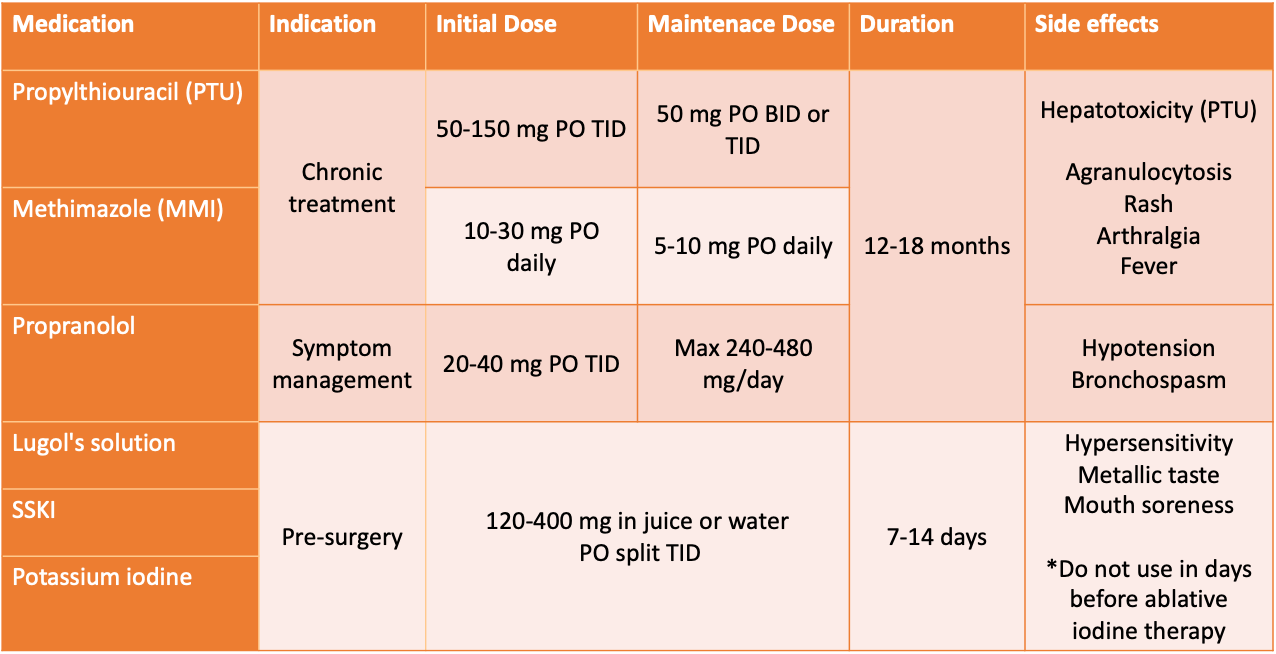
3b. Nonselective beta-blockers
- Non-selective beta blocker: propranolol
- Mechanism: blocks many hyperthyroidism symptoms mediated by beta-adrenergic receptors and may block T4 conversion to T3 at high doses
3c. Iodines and iodides
- Medications: Lugol's solution, saturated solution of potassium iodide (SSKI), potassium iodide tablets
- Mechanism: inhibits release of stored thyroid hormone; helps decrease vascularity and size of gland before surgery
- Limited efficacy after 7-14 days; primary use is before surgery to shrink the gland or after ablative therapy (3-7 days) to inhibit thyroiditis-mediated release of store hormone. Can be used acutely in thyroid storm (see subsection below).
Subclinical Hyperthyroidism
This occurs when there is a low or undetectable TSH, but a normal T4 level.
The risk of subclinical hyperthyroidism is associated with:
- Elevated risk of atrial fibrillation in patients 60+ years old
- Elevated risk of bone fracture in postmenopausal women
Treat with oral thioureas or beta blockers (may help control CV mortality).
If left untreated, the patient can develop overt hyperthyroidism.
Thyroid Storm
This is a severe and life-threatening state of thyrotoxicosis. The mortality rate is estimated at 20%. Thyroid storm is usually precipitated by trauma, infection, abrupt withdrawal of antithyroid agent, or inadequate pretreatment for post-ablative therapy.
Symptoms: fever, tachycardia, vomiting, dehydration, coma, tachypnea, delirium
Treatment algorithm (steps 1-5):
- Thiourea --> PTU 500-1000 mg loading dose, then 250 mg every 4 hours --OR– MMI 60-80 mg daily to block new hormone synthesis
- Iodide therapy 1 hour after PTU or MMI to block hormone release
- Beta-blocker (propranolol or IV esmolol) for symptom control
- Acetaminophen as needed for fever (AVOID NSAIDs due to displacement of protein-bound thyroid hormones)
- Steroids --> Prednisone 300 mg IV loading dose, then 100 mg every 8 hours (or appropriate prednisone equivalent for load and maintenance dose) to prevent adrenal insufficiency and block conversion of T4 to T3.
Hypothyroidism
There are less mechanisms for hypothyroidism, and many of them are due to an iodine deficiency. Approximately 30% of the world's population is still at risk for iodine deficiency. This rate has continually decreased over the past few decades due to the production and consumption of iodized table salt.
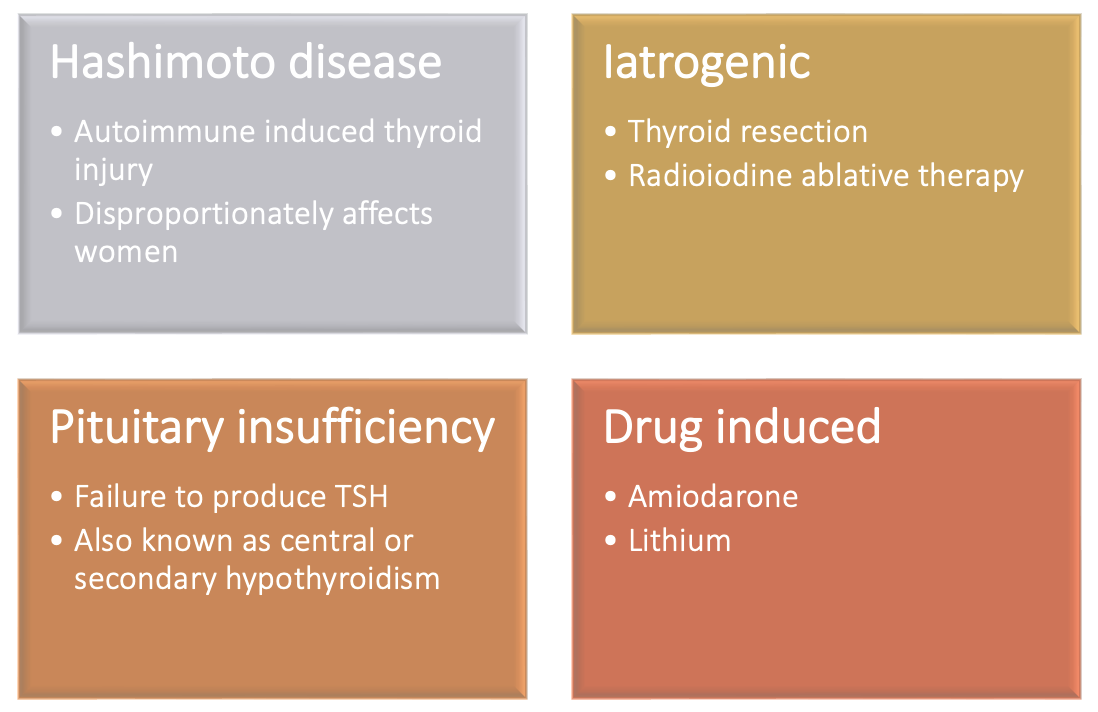
Diagnosis
Laboratory values indicative for hypothyroidism include:
- Low free T4
- Elevated TSH (usually >10 mIU/L) (TSH is normal or low if central hypothyroidism is the cause)
- Presence of antithyroid peroxidase antibodies or antithyroglobulin autoantibodies
Presentation
As you might expected, the symptoms of hypothyroidism are almost opposite from what we discussed with hyperthyroidism. Symptoms of HYPOthyroidism: cold intolerance, dry skin, fatigue, weight gain, bradycardia, slow reflexes, coarse skin and hair, menstrual disturbances, goiter
Treatment
1. Levothyroxine (drug of choice!)
- Mechanism: synthetic T4 to supplement the lack of T4 and T3 in circulation
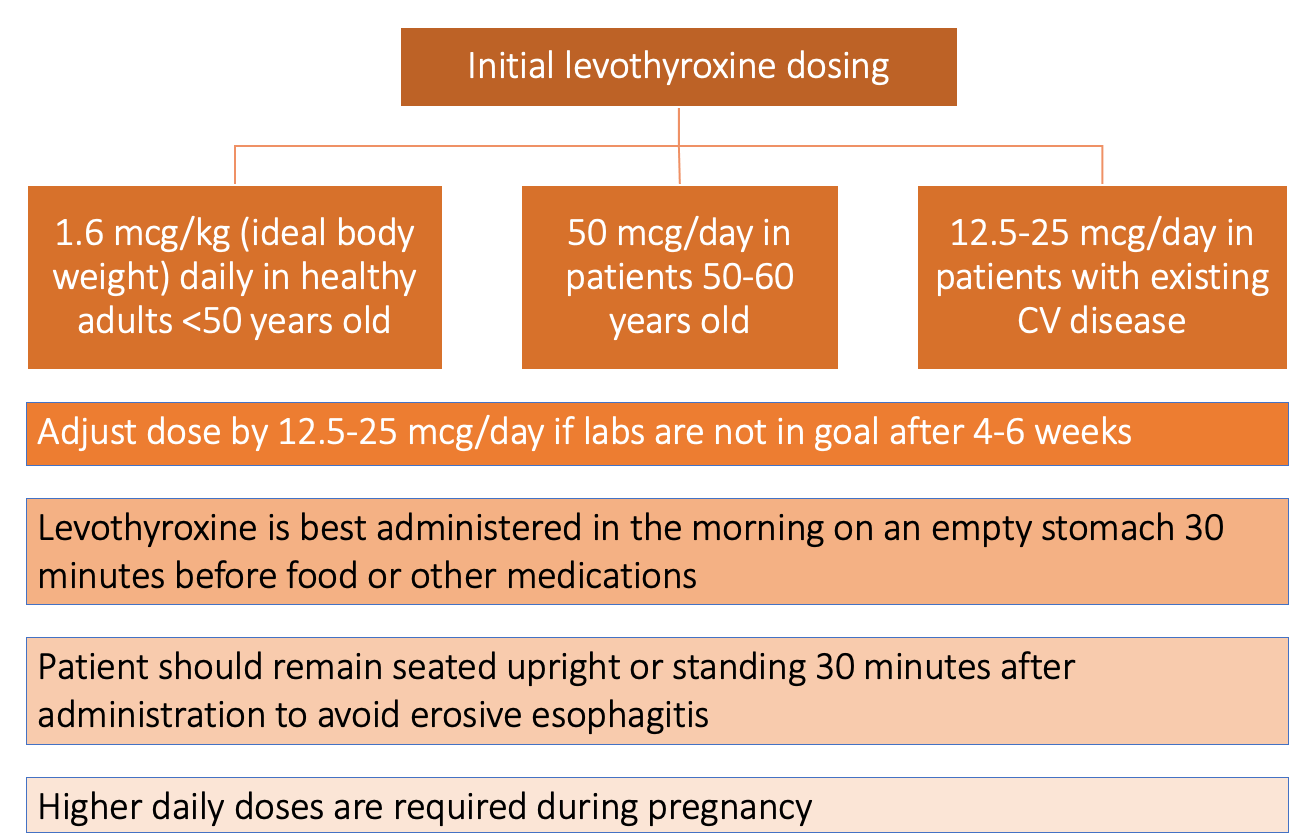
- Monitoring: it will take 4-6 weeks to see a change in thyroid panel values after starting or changing the dose of levothyroxine. Use free T4 rather than TSH if treating central or secondary hypothyroidism.
- Levothyroxine is a lifelong medication required to maintain TSH and free T4 in normal ranges.
- The American Association of Clinical Endocrinology (AACE) recommends brand name levothyroxine (Synthroid) over other formulations. Brand/generic levothyroxine switches are not bioequivalent and the prescribing provider should be contacted if a switch in products is required.
2. Other pharmacotherapy products
- Liothyronine: synthetic T3
- Liotrix: synthetic T4/T3
- Desiccated thyroid
- **None of the above are recommended due to variability in T4 and T3 concentrations
Subclinical Hypothyroidism
This occurs when there is an elevated TSH with normal T4 level.
The risk of subclinical hypothyroidism is associated with:
- Elevated risk of heart failure in older adults if TSH greater than 7.0 mIU/L
- Elevated risk of coronary heart disease if TSH greater than 10 mIU/L
Treatment of subclinical hypothyroidism is controversial as the benefit in some patients is inconclusive.
When to treat: TSH 4.5-10 mIU/L and,
- Symptoms of hypothyroidism
- Antithyroid peroxidase antibodies present
- History of CV disease, heart failure, or risk factors for either
Give initial daily dose of 25-75 mcg PO.
If left untreated, the patient can develop overt hypothyroidism (Hashimoto disease).
Myxedema Coma
This is a severe and life-threatening state of hypothyroidism. The mortality rate is estimated at 30-60%. Myxedema coma is usually precipitated by trauma, infection, heart failure, or medications (sedatives, narcotics, anesthesia, lithium, amiodarone).
Symptoms: altered mental state, diastolic hypertension, hypothermia, hypoventilation
Treatment:
- Intravenous thyroid hormone replacement with T4 200-400 mcg loading dose then 1.6 mcg/kg daily until able to take PO.
- Antibiotic therapy should be given if underlying infectious cause.
- Steroids --> Hydrocortisone 100 mg every 8 hour (or appropriate hydrocortisone equivalent). Steroids can be discontinued if random cortisol concentration is not depressed.
Clinical practice perspective from an inpatient hospital pharmacist:
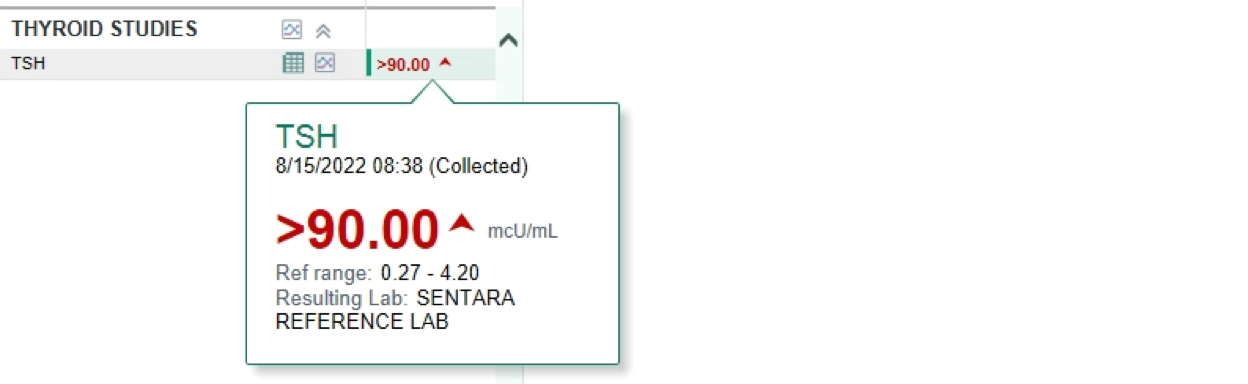
In the acute inpatient setting, chronic thyroid treatment is important to be reconciled and continued, but is not typically a primary problem upon patient presentation. However, there are times when a thyroid panel is collected and an imbalance in thyroid homeostasis is identified. Below is a TSH that resulted in an older female patient that was weak, fatigued, and had gained 10 pounds over the passed year unintentionally. These symptoms are consistent with that of hypothyroidism. An elevated TSH + undetectable T4 (not shown here) led to the initiation of levothyroxine during admission.
Sometimes, thyroid disorders are not identified until a hospital encounter, as some primary care providers do not collect these labs in their practice without clear signs and symptoms. Thyroid disorders can be found on "accident" in the hospital.
However, TSH, T4, and T3 values can be altered from other factors such as adrenal insufficiency, medications, euthyroid sick syndrome, etc. It is important to take into consideration what other factors the patient has upon presentation. Patients may not require immediate treatment with thyroid pharmacotherapy, as there may be an acute, temporary elevation/depression in TSH. A thyroid panel should only be obtained if there is a clinical suspicion for thyroid abnormalities. I plan to write another RxTeach article on this specific topic in the future!
References:
- Kane MP, Bakst G. Thyroid disorders. In: DiPiro JT, Yee GC, Posey L, et al., eds. Pharmacotherapy: A Pathophysiologic Approach, 11th ed. New York: McGraw-Hill, 2020.
- Rahn R, Burch H, Cooper D, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Endocr Pract 2011;17:e1-65.
- Garber J, Cobin R, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid 2012;22:1200-35.

