Let's Iron This Out: Controversies in Iron Therapy!
Many controversies exist with iron supplementation in the medical field. We walk through infection risk, use in heart failure, chronic kidney disease, and more!

We asked, you answered!
If you follow us on Instagram, you may have voted in our poll a while back. The poll asked if you would be interested in a post about iron therapy management! The results were pretty unanimous:
In this post, we will briefly cover some of the outlined objectives from my Continuing Education presentation, and paid subscribers will have access to the full PowerPoint slide deck as well as a recording of the presentation itself!
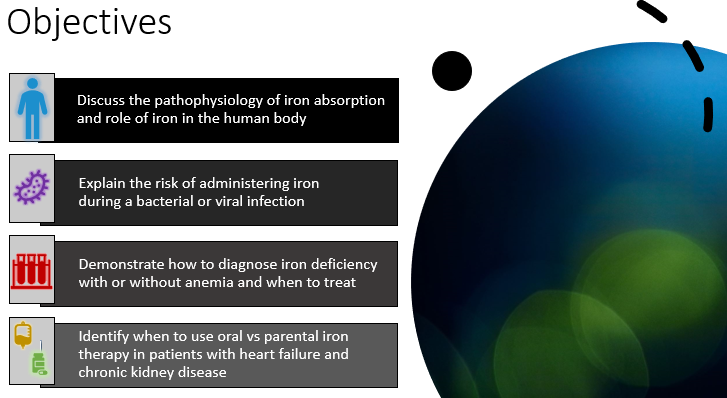

Objective 1: Iron Absorption and the Role of Iron
Iron is incredibly important for human physiology! Specifically, iron is involved in:
- Detoxification
- DNA synthesis
- Electron transport
- Energy metabolism
- Mitochondrial energy transport
- Oxygen transport
- Thyroid metabolism
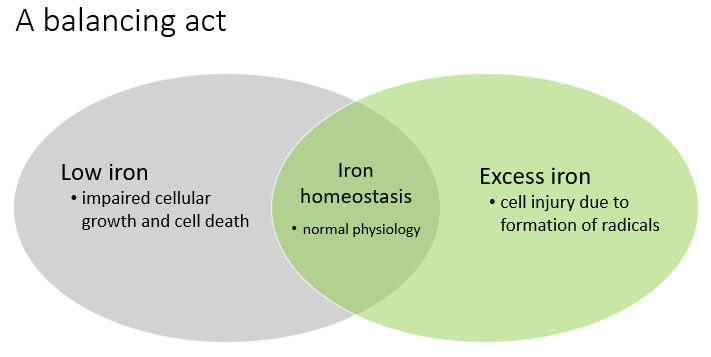
There is no elimination method for iron in the human body. Iron homeostasis is regulated by rate of absorption and iron release from storage sites in cells and tissues.

Objective 2: Iron and Infection Risk
We will first address what role iron has in immunity. Iron molecules can become oxidized, form iron radicals, and kill bacteria. However, bacteria can also use free iron molecules in the blood stream to aid in reproduction. See the graphic below for a visual representation.
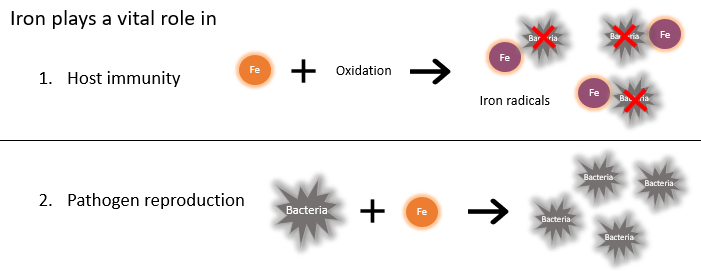
This means we must be careful to not overload a patient with iron. This is especially important when the patient has an active infection or uncontrolled source of infection.
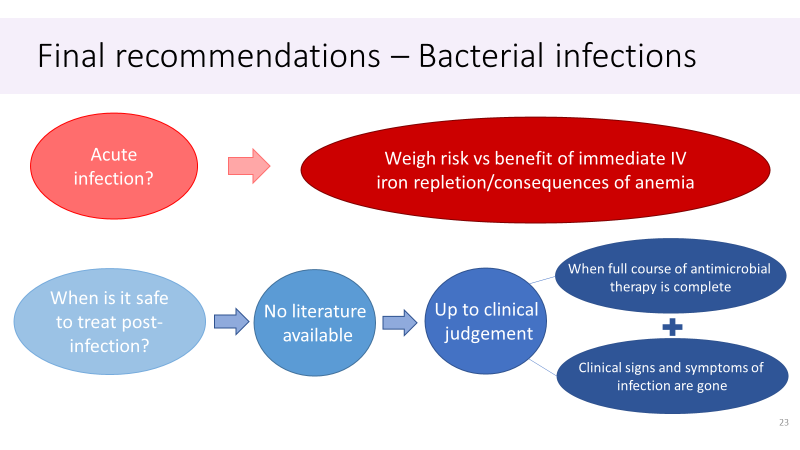
In theory, this makes sense. As you know, we are evidence-based medicine providers here at RxTeach! What does the literature say about the risk of iron repletion in patients who have an active infection?
CKD population: The KDIGO (Kidney Disease Improving Global Outcomes) 2012 Guideline for Anemia in Chronic Kidney Disease (CKD) recommends a trial of IV iron in CKD patients on HD and a 1-3 month trial of oral iron in non-HD CKD patients after the exclusion of active infection (2C recommendation).
Non-CKD population (i.e. all other patients): The data is more conflicting. In the full PowerPoint, I include a table that breaks down multiple meta-analyses. Shah et al 2021 published a meta-analysis in JAMA that is discussed in depth in the full presentation. Subscribe to RxTeach for access! For the purposes of this article, I will share the following figure:

Objective 3: Diagnosing and Treating Iron Deficiency
There are three definitions we need to talk through before diving into diagnosis and treatment. They are anemia, iron deficiency (ID), and iron deficiency with anemia (IDA).
Definitions!
Anemia (in adults) is when:
- Hematocrit: <42% (men) and <37% (females)
- Hemoglobin: <14 g/dL (men) and <12 g/dL (women)
Iron deficiency (ID) is when:
- Mean corpuscular volume (MCV) <80
- Red Blood Cell Distribution Width (RDW) >15%
- Low ferritin, Transferrin Saturation (TSAT), serum iron, and a high Total Iron Binding Capacity (TIBC)
Iron deficiency with anemia (IDA) is when:
- Low H/H + deficient iron labs!
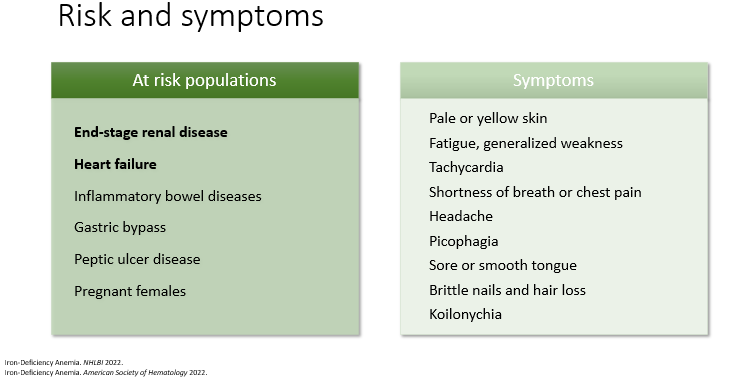
ID can cause depression, increased demand on the heart, increased risk for infections, cognitive delays, and pregnancy complications.
Diagnosing ID and IDA requires presence of symptoms and lab work (CBC, iron panel). See the full PowerPoint for a helpful flow diagram.
Treatment depends on the severity of symptoms, patient specific factors, and DOES NOT depend on the presence of anemia.
- For example, I have borderline iron deficiency anemia (IDA). I have known this for years when I would go to donate blood and my hemoglobin would be too low to donate. I started taking an iron supplement and eating better, and now my most recent H/H values (collected October 3, 2023) are within normal limits (see below).
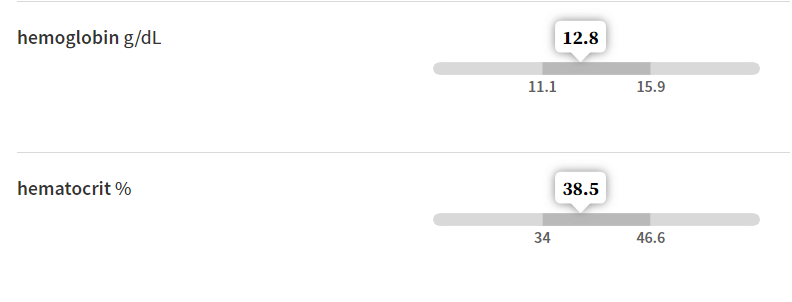
- However, I asked for these labs from my OBGYN because I recently have been feeling fatigued, cold, and bruise relatively easily. I do not have IDA because my H/H are within normal limits, but what about my iron labs? Turns out my ferritin was okay as well. On the lower end of the spectrum (<30 would be considered ID), my ferritin of 51 is not reason for diagnosis of ID, but shows me that maybe I should be more consistent on taking my daily multivitamin with iron!
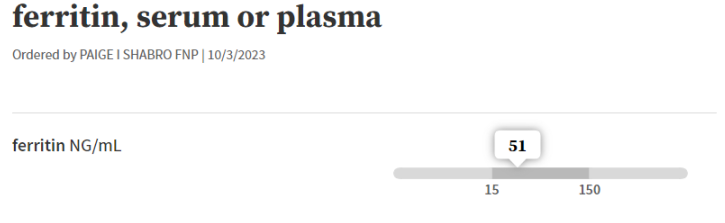
- My point here is that even though I do not have IDA or ID (officially), I was experiencing symptoms and may benefit from an OTC iron supplement and follow-up in a year for repeat labs if my symptoms do not improve.
Treatment cont.
Okay! Back to the presentation content. If you do have a patient with IDA or ID, oral iron supplementation is the place to start. Note that it will 3-6 months to replete stores.
Consider Intravenous Iron supplementation if:
- Severe anemia or severe symptoms are present
- Comorbidities limit expected absorption of PO iron
- The patient has not tolerated/responded to PO therapy previously
*Please refer to the PowerPoint for a table of available oral and IV iron products, how to dose oral iron (based on Kaundal et al 2020), and duration/monitoring of therapy.

Objective 4: Oral vs Parenteral Iron in HF and CKD
This last objective is when the presentation becomes literature HEAVY. There are multiple key trials recently published and currently ongoing relating to this topic.
Intro to ID in HF and CKD
Heart Failure (HF)
- Estimated >50% prevalence of ID in this population
- ID is a strong indepdent predictor of HF outcomes
- Treat ID in HFrEF if ferritin <100 ng/mL or ferritin 100-300 ng/mL AND TSAT <20%
Chronic Kidney Disease (CKD)
- Major driver of anemia in CKD is erythropoietin deficiency
- ID is a prominent contributing mechanism in impaired erythropoiesis
- Risk factors for ID/IDA in CKD: blood loss, chronic inflammation, impaired iron absorption
Guideline/Literature recommendations for ID in HF
The 2017 ACC/AHA/HFSA Heart Failure Focused Update from JACC do not make a distinction between preserved and reduced ejection fraction in their anemia recommendation:
- "In patients with NYHA class II and III HF and ID (defined above), IV iron replacement might be reasonable to improve functional status and quality of life. (2b recommendation)
- The 2021 Update to the 2017 Guidelines list Anemia and ID separately:
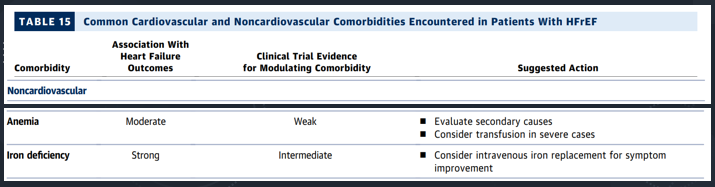
**See the full PowerPoint for a table on the following clinical trials that led to these recommendations (CONFIRM HF 2015, EFFECT HF 2017, IRONOUT 2017, AFFIRM 2020). These studies included patients with reduced EF.
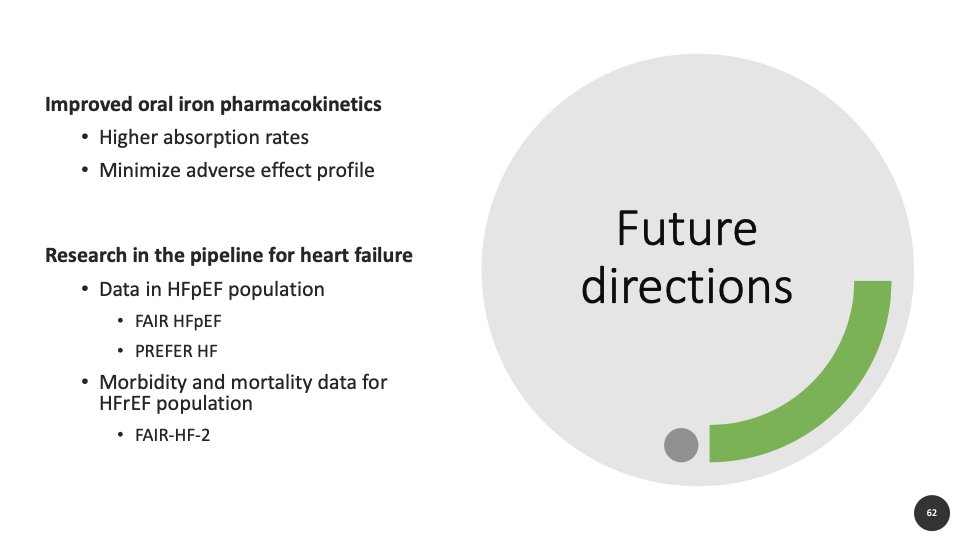
Key takeaway: The studies found that high-dose PO iron did not increase exercise capacity but did increase hemoglobin. Meanwhile, IV iron increased exercise capacity, QoL, NYHA class, and hemoglobin. The AFFIRM 2020 was the first trial to show that IV iron supplementation reduced hospitalizations in patients with LVEF <50% and who were stabilized after an episode of acute heart failure. Note, there is no data on mortality at this time.
Regarding patients with HFpEF, there is limited data from meta-analyses, no RCTs, and it is thought that ID may play an important role in this population, but there is no robust data at this time.
Iron Therapy Recommendations in HF
1. Treat ID with or without anemia
2. Replete with IV if HFrEF (EF <50%). Recommend iron panel for:
- Patients admitted with acute HF exacerbation w/o an iron panel in previous 6 months
- Patients w/ history of HFrEF admitted for another indication and there is clinical suspicion of ID based on signs/symptoms ± iron panel in previous 6 months
3. HFpEF
- Treat if symptomatic, and check an iron panel if no previous labs in last 6-12 months
- Trial oral iron first, recheck iron panel in 6-8 weeks, then recheck q6-12 months when stable
Patients with CKD
Iron Therapy Recommendations in CKD-HD
KDIGO 2012:
- Trial of iron for TSAT </= 30% and ferritin </= 500 ng/mL
European Renal Best Practice 2013:
- Trial of iron for TSAT <20% and ferritin levels < 100 ng/mL
National Institute for Healthcare and Excellence 2015 and the Renal Association 2017:
- Increase ferritin ceiling to 800 ng/mL due to more evidence that many patients with CKD have ferritin levels >500 ng/mL
Iron Therapy Recommendations in CKD Non-HD
No guideline recommendations.
Key trials discussed in the full presentation:
- FIND-CKD 2014
- REVOKE 2015
- PIVOTAL 2021
Key Takeaways:
- Trial of oral iron if ferritin <500 ng/dL and TSAT <30%, or symptomatic from ID
- Recheck iron panel in 6-8 weeks
- Check q6-12 months when stable
Summary
- Iron is involved in growth, development, and host immunity
- Mixed literature on infection risk with iron, and clinical judgement should be used on severity of symptoms ± anemia and patient specific factors
- Consider iron deficiency in the differential diagnosis for unexplained symptoms and treat regardless of presence of anemia
- HFrEF and CKD-HD most likely require IV iron
- HFpEF and CKD-ND consider trial of oral iron first
References
References are linked throughout the article and included at the bottom of each slide in the full PowerPoint deck.
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.

