DeLLphi-304 Journal Club
Compared to chemotherapy, tarlatamab showcased improved efficacy and safety following progression on or after platinum-based therapies.

Continuing from my last journal club article covering the IMforte clinical trial, today I will be breaking down the DeLLphi-304 trial and how it impacts the current treatment paradigm of small-cell lung cancer.
The DeLLphi-304 clinical trial was published in the New England Journal of Medicine in July 2025. Today, we will break down the trial and discuss its impact on clinical oncology treatment.
Background/Overview
Title: Tarlatamab in Small-Cell Lung Cancer after Platinum-Based Chemotherapy
Citation: Mountzios G, Sun L, Cho BC, et al. Tarlatamab in Small-Cell Lung Cancer after Platinum-Based Chemotherapy. N Engl J Med. 2025;393(4):349-361. doi:10.1056/NEJMoa2502099
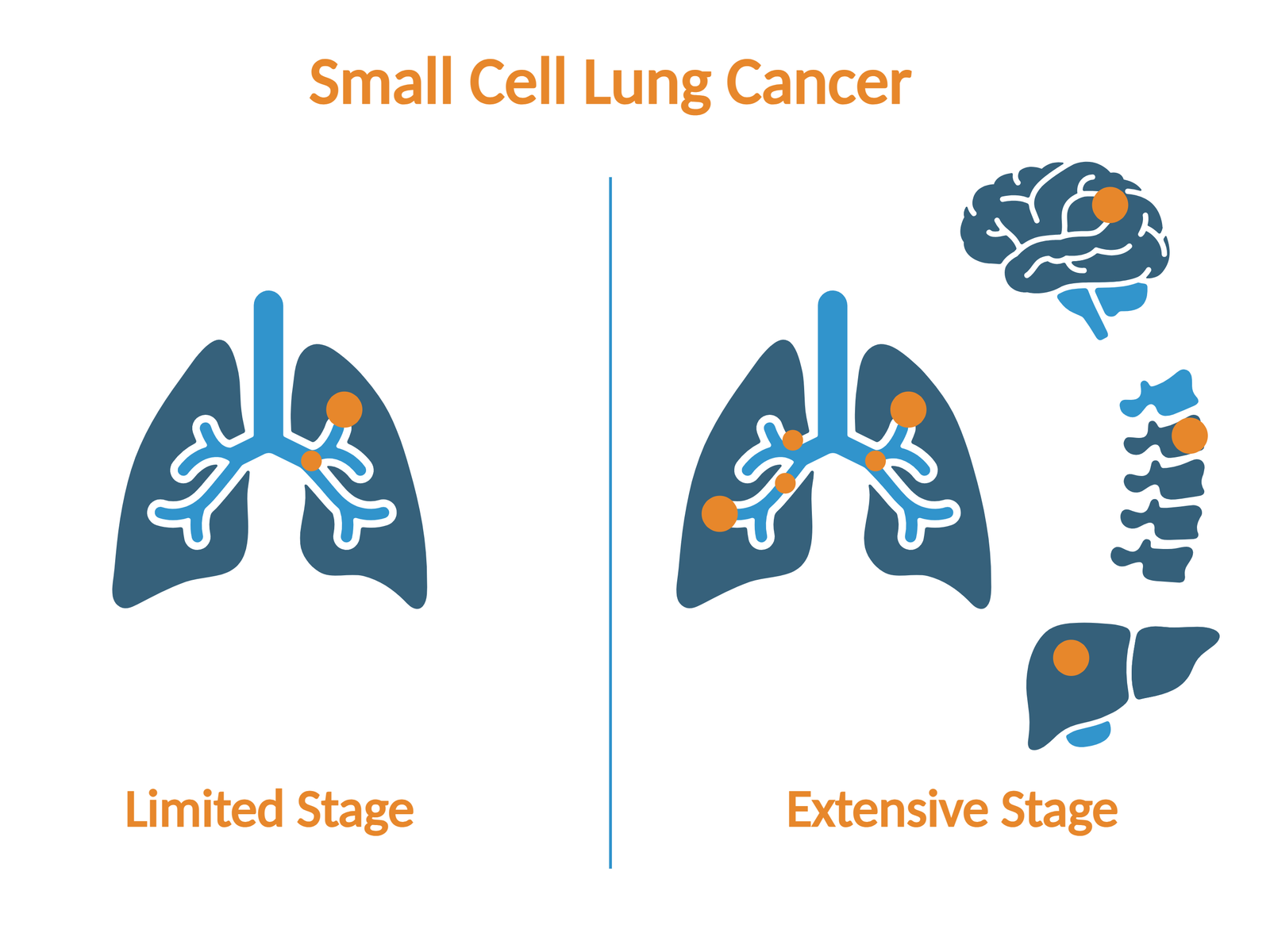
Background: Small-cell lung cancer is difficult to treat, with high rates of relapse/progression on first-line therapies. In the second-line setting, progress has been limited, with current options including topotecan, lurbinectidin, and amirubicin, depending on which country you live in. From the authors, lurbinectiden and amirubicin have not shown markedly longer overall survival in phase 3 trials and are associated with notable hematologic toxicities. This highlights the need for improvements in both the efficacy and safety of 2L options in this challenging disease.
Objective: To compare the efficacy and safety of tarlatamab versus standard of care chemotherapy following progression on platinum-based chemotherapy in the treatment of small cell lung cancer
Primary Efficacy Measure: Overall Survival (OS)
Key Secondary Efficacy Measure(s): Investigator-assessed progression-free survival (PFS), confirmed objective response, duration of response (DOR), and patient-reported outcomes
There were additional secondary and exploratory endpoints, but they will not be discussed to remain concise*
Participants:
- 18 years of age or older
- Cytologically/histologically confirmed small cell lung cancer
- Progression of disease after 1st line treatment with platinum-based chemotherapy with or without the use of immune checkpoint inhibitors
- Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1
- Asymptomatic, treated or untreated clinically stable CNS metastases
- Symptomatic CNS metastases
- Active autoimmune disease
Design: Multinational, multicentre, phase 3, open-label trial
Intervention: Patients were randomly assigned in a 1:1 ratio to receive:
- Experimental group (254 patients): Tarlatamab, a bispecific T-cell engager targeting Delta-like ligand 3 on tumor cells and CD3 on T-cells
- Tarlatamab was administered as a 60-minute IV infusion initiated with a step-up dose of 1 mg on day 1 of cycle 1, followed by 10 mg on days 8 and 15 of cycle 1, and then 10 mg every 2 weeks in 28-day cycles.
- Control group (255 patients): physician's choice of chemotherapy (185 (73%) received topotecan, 47 (18%) lurbinectedin, and 23 (9%) amrubicin) administered in 21-day cycles
- Topotecan was given IV at 1.5 mg/m2 (except in China, where 1.2 mg/m2 was used) or orally at a dose of 2.3 mg/m2 on days 1 through 5 every 3 weeks
- Lurbinectedin was given IV at 3.2 mg/m2 on day 1 every 3 weeks
- Amirubicin was given IV at 40 mg/m2 on days 1 through 3 every 3 weeks
Stratification factors:
- Previous exposure to PD-1/L1 inhibitors (Y/N)
- Chemotherapy-free interval (<90 days, ≥90 to <180 days, or ≥180 days)
- Presence of brain metastases (Y/N)
- Intended chemotherapy (topotecan or amrubicin vs. lurbinectedin).
*Administration of treatments continued until disease progression, according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1; unacceptable toxicities; withdrawal of consent; or death. Continuation of trial treatment after disease progression was allowed, provided the investigator determined clinical benefit.
Statistical Analysis: Sample size was based on the overall survival analysis. With a 2-sided α-level of 0.05, with approximately 345 deaths among 490 patients between the two treatment arms, 91% power would be attained to detect a hazard ratio for death of 0.70
- Overall survival was analyzed in an intention-to-treat analysis, including all patients who were randomized, and utilized the Kaplan-Meier method to estimate the survival distribution
- Safety outcomes were assessed by treatment received and included patients who had received at least 1 dose of the trial treatment

Results
Enrollment occurred between May 31, 2023, and July 30, 2024. 688 patients were assessed for eligibility across 166 sites in 30 countries, and 509 were included. Data cutoff date: January 29, 2025
Baseline demographics:
Median age: 65 years (range, 20 to 86)
Female: 31%
ECOG PS 1: 67%
Current/former smoker: 89%
Brain metastases (current or previous): 45% at baseline
Liver metastases: 35%
Previous PD-1/L1 therapy: 71%
Platinum-resistant disease: 44%
*The median duration of treatment was 4.2 months with tarlatamab and 2.5 months with chemotherapy. 27% and 7% were still receiving treatment at data cutoff, respectively.
mOS 13.6 months vs 8.3 months. Stratified HR for death was 0.60 (95% CI, 0.47 to 0.77; P<0.001)
Overall survival was 76% at 6 months and 53% at 12 months vs 62% at 6 months and 37% at 12 months in the chemotherapy group
*Median follow-up for OS was 11.2 months in the treatment group and 11.7 months in the control
mPFS was 4.2 months vs 3.7 months (HR, 0.72 [95% CI: 0.59 to 0.87]; P < 0.001)
Confirmed objective response was 35% vs 20% (risk ratio, 1.73; 95% CI, 1.29 to 2.33)
Median DOR was 6.9 months vs 5.5 months. Kaplan-Meier estimate of 12-month DOR was 41% vs 13%
Patient-reported changes at week 19:
Tarlatamab saw significant reductions in dyspnea symptom scores vs chemotherapy (mean between-group difference, -9.14 points; 95% CI, -12.64 to -5.64; P<0.001) as well as cough (odds ratio for decrease in cough score, 2.04; 95% CI, 1.17 to 3.55; P=0.01; risk ratio for decrease in cough score, 1.74; 95% CI, 0.99 to 2.49).
The between-group difference in chest pain score was not significant (odds ratio for decrease in chest pain score, 1.84; 95% CI, 0.89 to 3.81; risk ratio for decrease in chest pain score, 1.81; 95% CI, 0.54 TO 3.08
Grade 3 or higher AEs: 54% vs 80%
Treatment-related AEs (TRAEs): 93% vs 91%
Grade 3 or higher TRAEs: 27% vs 62%
Most common grade 3 or higher TRAEs with tarlatamab:
neutropenia (4%), lymphopenia (4%), decreased lymphocyte count (3%), fatigue (in 2%), decreased neutrophil count (2%), hyponatremia (2%), and anemia (2%)
Most common grade 3 or higher TRAEs with chemotherapy:
anemia (28%), neutropenia (22%), leukopenia (14%), febrile neutropenia (11%), thrombocytopenia (11%), and neutrophil count decrease (11%)
TRAEs leading to dose interruption, reduction, or both: 19% vs 55%
TRAEs leading to discontinuation of treatment: 3% vs 6%
TRAEs leading to death: 1 patient (<1%) vs 4 patients (2%)
Cytokine release syndrome (CRS) occurred in 56% of the tarlatamab-treated patients (42%, grade 1; 13%, grade 2; 1%, grade 3; no grade 4 or 5 CRS events reported)
Immune effector cell–associated neurotoxicity syndrome (ICANS) occurred in 6% of the tarlatamab-treated patients
(All the events were assessed as grade 1 or grade 2, except for one event of grade 5)
Neurologic AEs: 56% vs 35%
-Dysgeusia was the most common neurologic AE in the tarlatamab group; incidence of 24% (18%, grade 1; 6%, grade 2), as compared with 2% in the chemotherapy group (all grade 1)
Strengths:
- Multicenter and international design
- Intention-to-treat analysis for efficacy endpoints
- Well-validated stratification factors
- Included those with brain metastases
- High proportion of patients with previous PD-1/L1 exposure
- High proportion of patients deemed platinum resistant
Limitations:
- Open-label/unmasked design, especially impacting patient-reported symptoms
- Inclusion criterion of only those with an ECOG performance status score of 0 or 1 decreases external validity
- Most patients in the chemotherapy arm utilized topotecan (73%), a 2L option shown not to be optimal in platinum-resistant disease
- Underrepresentation of some racial groups, including African Americans
Authors’ conclusions:
The results of the DeLLphi-304 trial showed superior efficacy of a T-cell engager therapy over chemotherapy in patients with small-cell lung cancer whose disease had progressed during or after first-line platinum-based chemotherapy

Cost (per Lexidrugs Online 2025): Tarlatamab (Imdelltra)
Solution (reconstituted) (Imdelltra Intravenous)
- 1 mg (per each): $1,800.00
- 10 mg (per each): $18,000.00
- This equates to roughly $37,800 in the first month of therapy, and $36,000 for subsequent months
Final Thoughts
- In the Dellphi-304 clinical trial, Tarlatamab as a 2L option in those who progressed on or after platinum-based chemotherapy showcased statistical and clinical significance in prolonging survival in small cell lung cancer patients and highlighted a manageable safety profile. Based on this data, tarlatamab has been incorporated as a category 1 preferred option in the NCCN guidelines. In my personal opinion, I am quite excited to see future research incorporating tarlatamab into earlier lines of therapy and assessing its impact.
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.

