Hot Takes on Hypertension
This post is a quick refresher on first-line treatment according to ACC/AHA 2017 Guidelines, plus helpful conversion charts!
This post is a quick refresher on first-line treatment according to ACC/AHA 2017 Guidelines for Management of High Blood Pressure in Adults, plus helpful conversion charts!
Disclaimer: This post is meant to provide an overview of a clinical topic that may include (but is not limited to) information on pathophysiology, diagnosis, treatment, clinical pharmacology, medication management, adverse effects, and clinical pearls. References are included at the bottom of each post. This post is not to be used as medical advice for direct patient care, but as a guide for learning and discussion.
Introduction
In 2010, high blood pressure (BP) was the leading cause of death and disability-adjusted life years worldwide. In the United States, hypertension (HTN) accounted for more cardiovascular disease (CVD) deaths than any other modifiable CVD risk factor. HTN was second only to cigarette smoking as a preventable cause of death for any reason! In 2020, more than 670,000 deaths in the United States had HTN as a primary or contributing cause.
Many adult patients with HTN have other CVD risk factors. Among US adults with HTN between 2009 and 2012:
- 15.5% were current smokers
- 49.5% were obese
- 63.2% had hypercholesterolemia
- 27.2% had diabetes
- 15.8% had chronic kidney disease
What is Hypertension (HTN)?
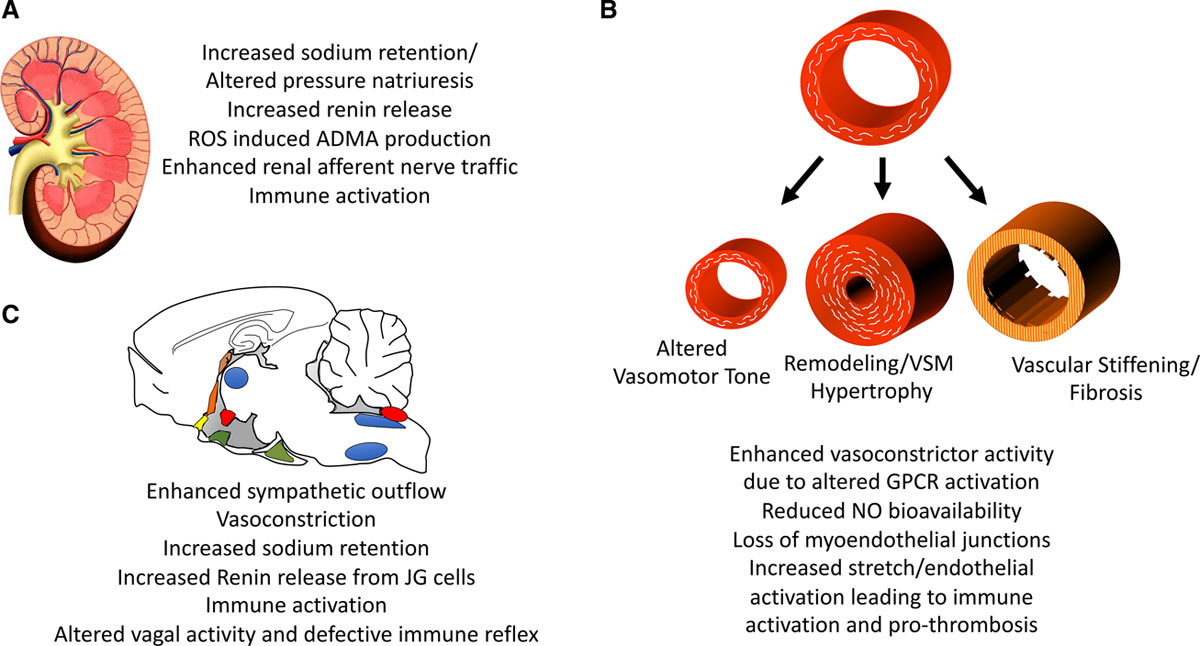
HTN is a condition in which the force of blood against the artery walls is too high. Figure 1 below shows the development of HTN over time and what factors can contribute to the pathophysiology.
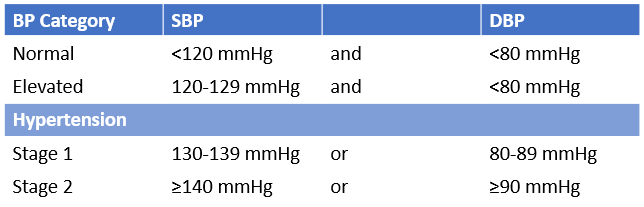
The ACC/AHA have provided clinical markers to identify elevated, stage 1, and stage 2 hypertension. Although a continuous association exists between increased CVD risk and higher BP, identifying patients based on the parameters below (Table 1) is useful in clinical practice when initiating antihypertensive medications.
In contrast, JNC8 2014 Guidelines have a flowchart approach for HTN management and treatment selection. In other words, they do not have defined stages/categories of HTN.
Something I was asked as a P4 student that I did not know: the blood pressure used for diagnosis of HTN is based on an average of 2+ readings obtained on 2 or more DIFFERENT occasions. If I would have read the guidelines more intently, I would have clearly seen this spelled out in their recommendations!
Another fun fact: higher SBP has been consistently associated with increased CVD risk. DBP has not shown this association.
How to diagnose/measure BP
Traditionally, the guidelines recommend measuring blood pressure when the patient has been sitting idle for >5 minutes in a chair with their back straight, feet on the ground, and arm at heart level. It is then suggested to use an average of ≥2 readings obtained on ≥2 occasions to estimate the individual’s level of BP.
However, a recent study presented at the American Heart Association (AHA) Hypertension Scientific Sessions 2022 in San Diego, California suggested that standing blood pressure readings, alone or in combination with seated BP readings, outperform seated BP readings alone for the initial diagnosis of HTN.
The most important point to remember when diagnosing someone with HTN is that multiple readings are critical. There are many factors that can acutely affect a patient's BP. Taking numerous readings on various days and in various settings (at home vs in-office) can help make an accurate diagnosis.
What environmental factors can affect HTN?
- Weight: more body weight is correlated with higher BP. There is an even stronger relationship between higher BP and waist-to-hip ratio.
- Sodium intake: directly related to higher BP and is independently associated with increased risk for stroke, CVD, and other adverse outcomes.
- Potassium intake: inversely related to elevated BP and stroke. A higher level of potassium seems to blunt the effect of sodium on BP.
- Physical fitness: inverse relationship with elevated BP and increased physical fitness.
- Alcohol: direct relationship; thought to account for about 10% of the population burden of HTN. The risk is higher in men than in women.
Treatment
Non-pharmacological recommendations
- Weight loss
- Heart healthy diet like DASH (Dietary Approaches to Stop Hypertension) diet
- Sodium reduction
- Potassium supplementation in the form of dietary modification (caution in renal and cardiac patients)
- Increased physical activity
- Limit alcoholic drinks to 2 a day for men and 1 for women
If your patients are wondering how much of a reduction in SBP they should see after implementing one or more of the above recommendations, Table 15 in the ACC/AHA guidelines lists an estimated value for each bullet above!
Pharmacological treatments
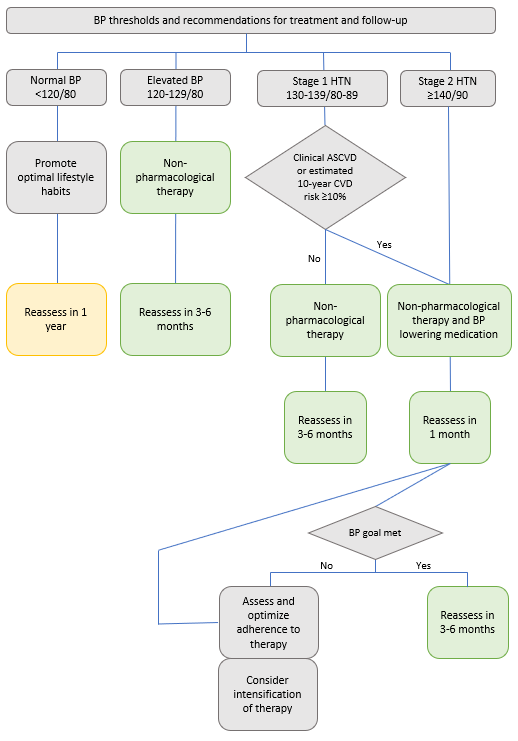
If a patient falls in Stage 1 or Stage 2 according to ACC/AHA, pharmacotherapy is recommended alongside non-pharmacological treatments (see Figure 2 below).
There are four first-line recommended medication classes for the treatment of HTN. They are:
- Dihydropyridine calcium channel blockers (DHP-CCBs)
- Thiazide diuretics
- Angiotensin converting enzyme inhibitors (ACE-Is)
- Angiotensin II receptor blockers (ARBs)
There are specifics on when one class should be preferred over another. Sometimes the disease state and/or race of the patient will help guide your recommendations. We talked about two key landmark trials that compare a few of the above medication classes against each other in our previous article from November 2022.
Along with deciding treatment options, monitoring frequencies must be determined. Figure 2 combines treatment selection and follow-up in one easy-to-use algorithm. This algorithm is built similarly to the flowchart in JNC8 (mentioned above).
Dosing strategies
So you have a patient with elevated blood pressure on 2 different occasions and want to start treatment. You know what first-line medication classes to use, but what dose should you start with? How many medications should you prescribe?
Typically in the outpatient/clinic setting, patients will not be in an acute HTN emergency/urgency (SBP >180mmHg +/- end organ damage). Therefore, you will have the luxury to start low and go slow with your treatment options.
The general consensus from the guidelines:
- Patients with Stage 1: initiate 1 antihypertensive agent
- Patients with Stage 2: initiate 2 antihypertensive agents
Let's say your patient has an average BP of 154/91 mmHg. They would fall in Stage 2 according to ACC/AHA. You decide to start 2 antihypertensive medications. A great option would be a combination tablet of 2 first-line options such as:
- amlodipine-hydrochlorothiazide (DHP-CCB/thiazide)
- benazepril-hydrochlorothiazide (ACE-I/thiazide)
- amlodipine-benazepril (DHP-CCB/ACE-I)
- losartan-hydrochlorothiazide (ARB-thiazide)
- the list goes on and on....
Combination tablets are great because it is less pill burden on the patient and sometimes preferred by insurance formularies!
Lets say we select amlodipine-benazepril. The recommended initial dose is amlodipine 2.5 mg/ benazepril 10 mg by mouth once daily. From there, we can reassess the patient every month or so and titrate up the dose until their BP is in goal (<130/<80 mmHg).
If you are in doubt, use a friend, check your references (looking at you Lexi-comp and Micromedex), and ask for help!
Dosing conversions
Many hospitals will have formularies that only carry a select few ACE-Is and ARBs. When a patient is admitted to your hospital, but they take a medication outpatient that is not on your formulary, a dose conversion must happen. With converting between various ACE-Is and ARBs, there will never be a clear black and white answer. It is important to take into consideration various factors. Remember, you are a clinical pharmacist and have to make clinical judgment calls that are in the best interest of the patient. The guidelines and dose conversion charts are not absolute, they are simply guiding you to a better final recommendation!
Various factors to consider when converting between medications:
- The patient's clinical status: are they septic on arrival? Are they currently hypotensive for another reason? Are they on other medications that would increase blood pressure? Did they recently go through a trauma that is causing hypertension? All of these could cause you to make a clinical judgment call to increase or decrease an anti-hypertensive dose instead of following a typical conversion chart as written.
- The patient's previous dose: what type of dose were they on outpatient? Were they on the max dose of benazepril or was it a small dose? What is the half-life of both medications in question (the home medication and the formulary medication)?
- The patient's allergies: are they allergic to ACE-Is and on an ARB outpatient? If yes, you better keep them on an ARB and not convert over to the formulary ACE-I. Were they on Entresto (sacubitril-valsartan) outpatient? If yes, be cautious about the 36-hour washout period for ACE-I initiation.
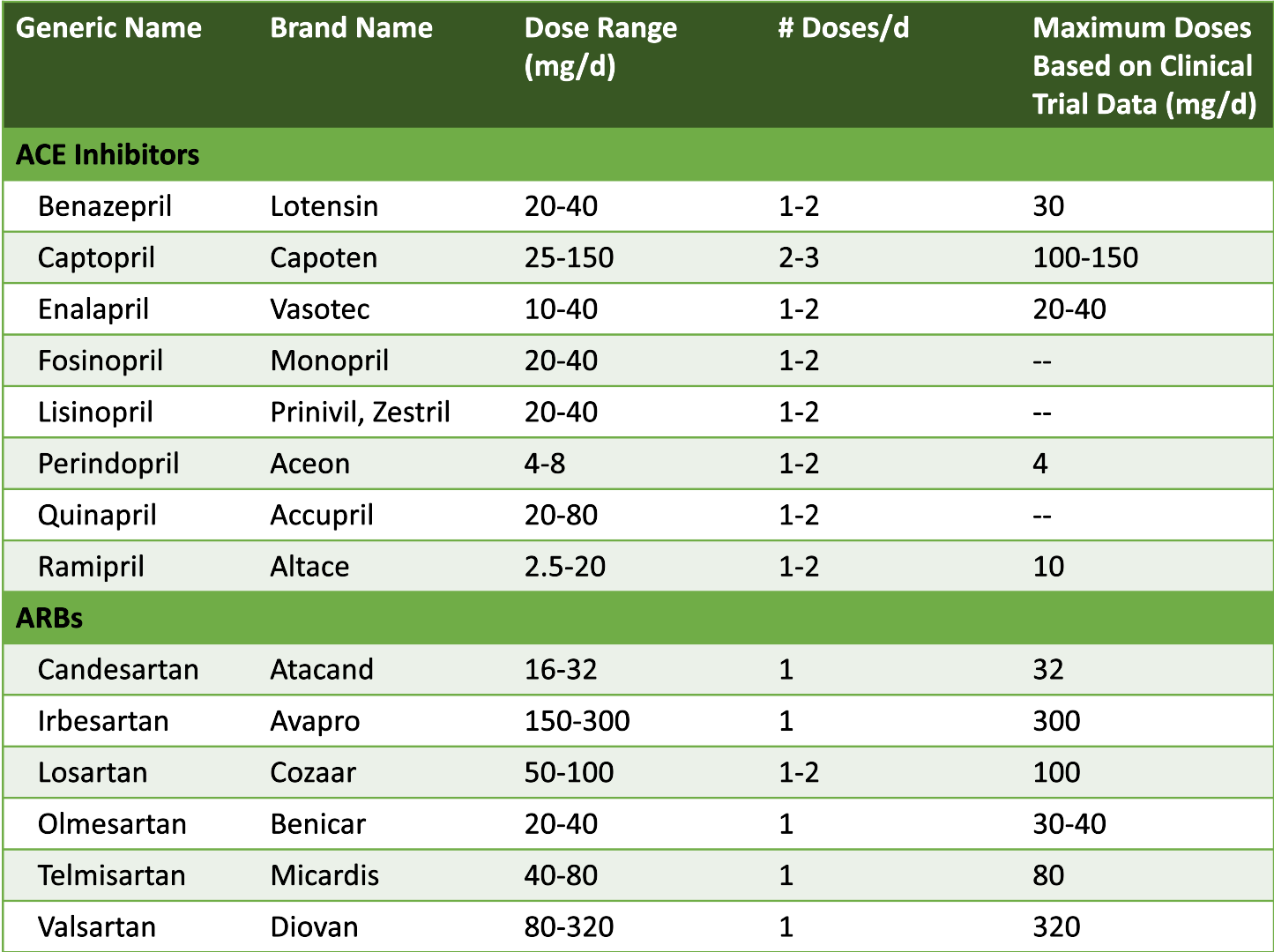
How to use Table 2. If a patient takes valsartan 80 mg once daily at home and the hospital formulary is losartan, what dose of losartan should you recommend? The dose range of valsartan in the chart is 80-320 mg/day. Currently, the patient is on a lower dose of valsartan. When looking at losartan, the dose range is 50-100 mg/day in one dose or split into two doses. To match the lower dose of valsartan, you will probably start with a 50 mg dose of losartan. You could recommend a once daily 50 mg order, or you could recommend 25 mg twice daily!
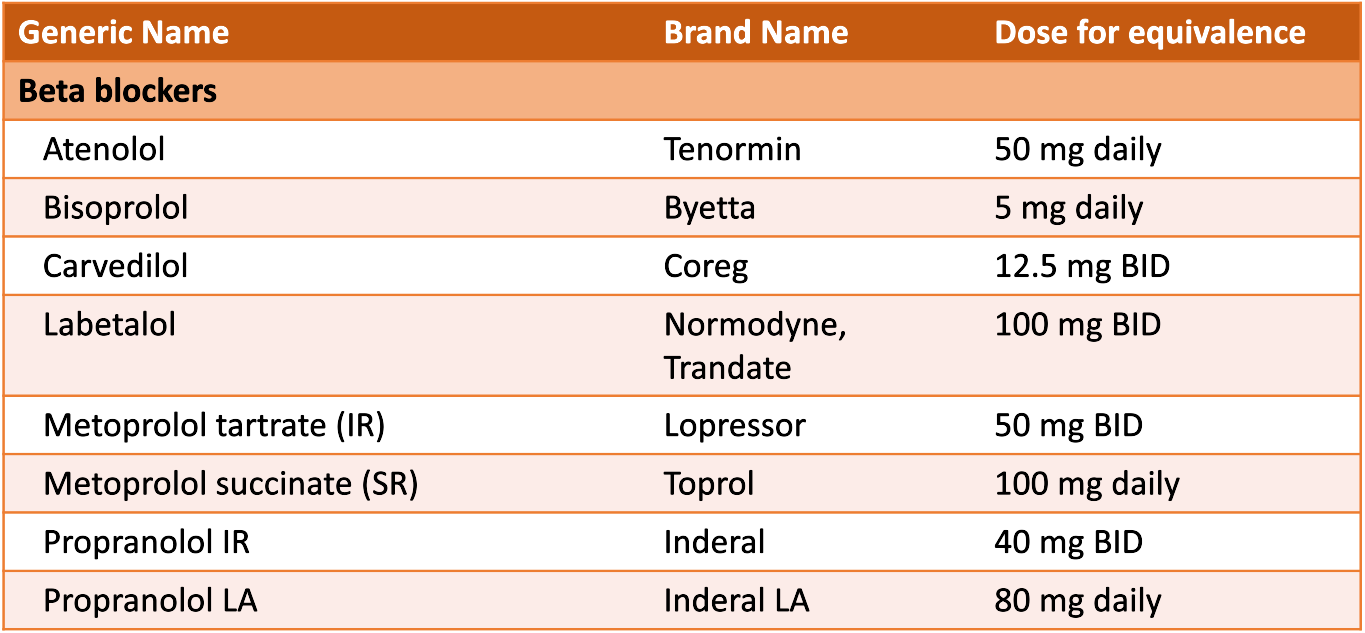
There are also conversion charts floating around the internet for beta-blockers. Depending on the patient's comorbid conditions, a beta-blocker can aid in lowering blood pressure as well. For example, ACC/AHA describe the following about beta blockers:
- Beta blockers are not recommended as first-line agents unless the patient has ischemic heart disease or heart failure (HF).
- [Cardioselective beta blockers] are preferred in patients with bronchospastic airway disease requiring a beta blocker: atenolol, bisoprolol, metoprolol.
- Bisoprolol and metoprolol succinate are preferred in patients with HFrEF.
Have a "hot take" about HTN that we did not discuss? Drop it in the comments below!

