Hypervolemic Hyponatremia
Hyponatremia in hypervolemic patients explained: risks in older adults, safe sodium correction, and treatment options including loop diuretics and vaptans.
Author: Dylan Hembrough, PharmD Candidate Class of 2028
Editor: Kristen Linduaer, PharmD, BCPS, AAHIVP
Hyponatremia, the condition of low sodium levels in the blood, is the most common electrolyte disorder.1,2 Defined as a serum sodium concentration of <135 mEq/L, it is estimated that 20-35% of all hospital patients experience hyponatremia1,2 It is usually asymptomatic, but quick changes in serum levels, or an extremely low serum level (<120 mEq/L), can lead to severe symptoms like seizures and coma.1
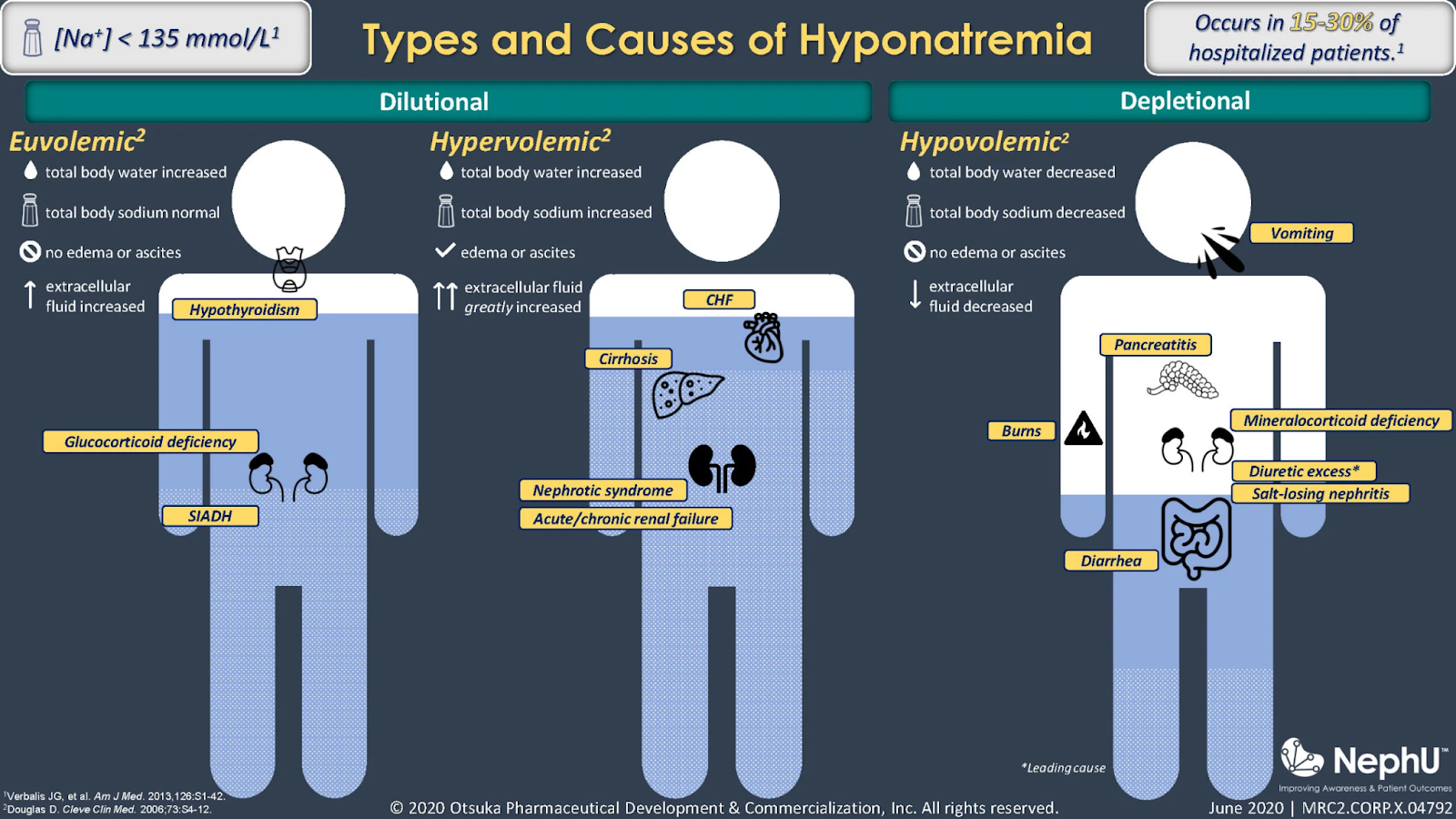
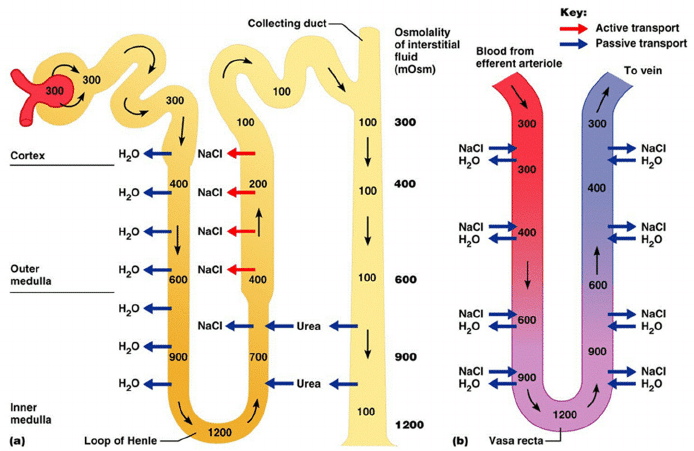
Graphic by NephU.
This disorder is often comorbid with hypervolemia, another common condition in which the body has taken on too much fluid. Serum sodium levels are closely intertwined with total body water, so hyponatremia tends to result from excess water rather than too little sodium.2 In other words: the more water there is, the more diluted the sodium in a person’s body.
Hypervolemia is also a common complication of congestive heart failure, and since more than 75% of congestive heart failure patients are over the age of 65, special consideration is often given to hypervolemia and hypervolemic hyponatremia in elderly patients.13 Due to other age-related complications, many medications will have exacerbated adverse effects in geriatric patients. These drugs are compiled in the Beers List.3
Hyponatremia itself is usually a secondary or tertiary concern. The primary concern is often fluid status changes, as fluid changes can lead to more tangible, acute effects. Since hyponatremia is often asymptomatic, it is easy to see why it is not the primary concern when treating a patient. However, there are likely connections between chronic hyponatremia and other risks or conditions that could be especially worrisome for geriatric patients. There is a link with cognitive impairment at serum sodium levels <132 mEql/L and gait disturbances at levels <134 mEq/L, which can increase the risk of falls and bone fractures.4
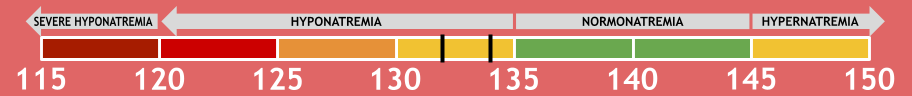
Graphic by Dylan Hembrough
Considerations Before Treatment
When correcting hyponatremia, small increases (3-7 mEq/L) are sufficient to reduce symptoms of hyponatremia and stop seizures.10 Correction should not exceed 8 mEq/L in 24 hours.10
The primary concern with sodium correction is osmotic demyelination syndrome, a condition where the protective sheaths around nerve cells are irreversibly damaged or destroyed. This occurs when serum sodium levels are corrected too quickly. The brain adapts to its new low-sodium environment after roughly 48 hours, so a rapid return to normal levels can “shock” the system and cause permanent nerve damage.2
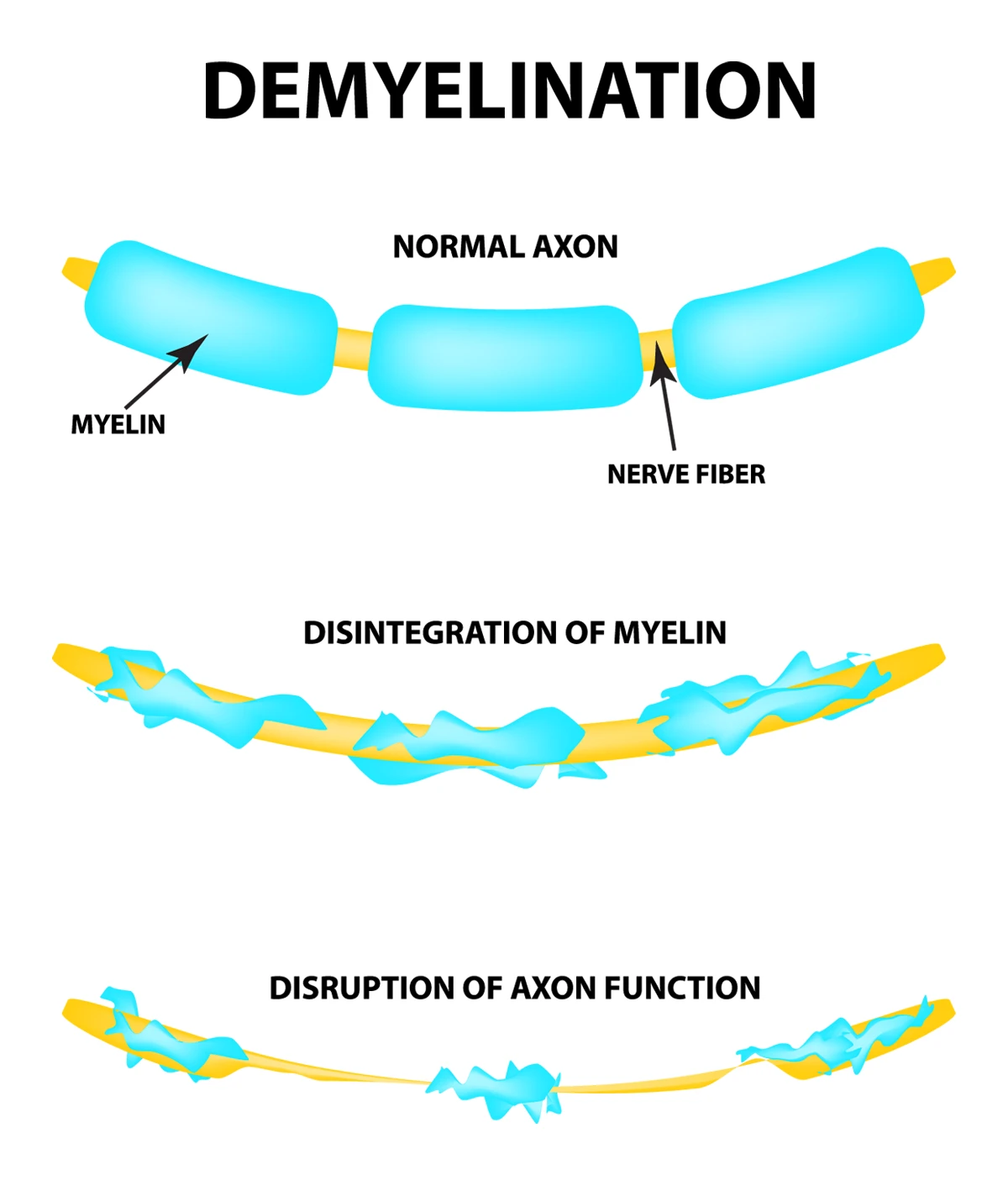
Graphic by Aurora Health Care.
Treatment Option 1: Loop Diuretics
Treatment of the underlying condition takes priority over direct treatment of hyponatremia, unless the patient’s hyponatremia is symptomatic.2 Initial treatment is to place the patient on fluid and salt restriction, as well as administer loop diuretics.2
Loop diuretics – namely furosemide, torsemide, and bumetanide – inhibit reabsorption in the loop of Henle in the kidney, resulting in increased water and sodium excretion.5 Loop diuretics are very effective and are a first-line treatment for hypervolemia.6 Also, loop diuretics do not appear on the Beers List, so no extra caution is needed when administering to geriatric patients.3
Graphic by DaVita Kidney Care.
However, loop diuretics do carry their own risks.
There is conflicting evidence as to whether or not the sodium-shedding activity of loop diuretics is significant enough to pose a challenge in the treatment of hyponatremia, since, ideally, the body is also proportionally shedding water.7 If the patient is being properly monitored, this would be an easy problem to identify.
There will be patients who exhibit diuretic resistance. Diuretic resistance occurs when, despite reaching the maximum dose of diuretic, fluid and sodium excretion are still insufficient.8 Furosemide, for example, is eliminated 100% renally, so patients with decreased kidney function (an eGFR of <30, according to LexiComp) may struggle to reap the benefits of this drug.
By and large, loop diuretics are the best available agents for this syndrome, but certain populations (patients with renal disease, patients who cannot be closely monitored, etc.) cannot be treated adequately with them. Fortunately, there are other treatment options for these patients.
Treatment Option 2: Vaptans
Selective vasopressin receptor 2 antagonists, also known as “vaptans,” have proven effective in patients without hepatic failure.2 They inhibit the action of vasopressin on renal collecting ducts and are primarily aquaretic, meaning they allow the body to shed water while retaining sodium.9 Vaptans are not on the Beers List either.3
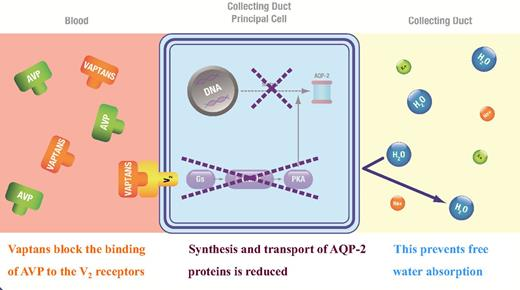
Graphic by A. Peri, et al.
Of course, vaptans also have their drawbacks. Their use is limited to 30 days due to adverse effects related to gastrointestinal bleeding and end-stage liver disease.6
Additionally, there was a case in 2014 where standing order tolvaptan therapy led to extreme hypernatremia and osmotic demyelination syndrome.9 In this case, it is important to note that, for some reason, tolvaptan therapy was continued even after blood panels indicated hypernatremia.9 Skepticism about the conclusions drawn from this case is certainly valid for that reason alone.9 Before the disastrous end result, the patient’s blood panels indicated that the therapy was working well.
Vaptans are certainly effective, but require a lot of close monitoring of serum sodium levels throughout treatment. So far though, vaptans have not dethroned loop diuretics as first-line therapy for this condition.
Other Treatment Options
In rare cases, use of a hypertonic intravenous solution may be indicated. Sodium chloride 3% is indicated only for symptomatic hyponatremia and must be monitored very closely, as it would be very easy to cause osmotic demyelination with too fast a serum sodium elevation.10
Oral sodium chloride therapy is also an option, but it isn’t used all that much in hypervolemic hyponatremia due to the water-retaining properties of sodium.12
Key Takeaways
Though hyponatremia usually isn’t the primary concern in hypervolemia, it is widespread in hypervolemic patients. If ignored, it may lead to unnecessary injury in the future, especially for older patients.
Loop diuretics are first-line therapy and generally effective in treating hypervolemic hyponatremia. In cases where they’re ineffective, vaptans can typically be used in their place.
Vaptans are a promising drug class and should be investigated further for use in this condition, especially due to the commonality of hyponatremia. As it stands, they should be used with caution and close monitoring.
Any sodium correction should be done slowly so as to prevent irreversible adverse effects. Small changes are enough to prevent the most severe symptoms of hyponatremia and enable the medical team to focus their efforts on solving other issues.
About the Author

References
1 Hyponatremia. Mayo Clinic. 2025 Jul 18.
5 Oh SW, Han SY. Loop Diuretics in Clinical Practice. Electrolyte Blood Press. 2015 Jun;13(1):17-21.
8 Wilcox CS, et al. Pathophysiology of Diuretic Resistance and Its Implications
for the Management of Chronic Heart Failure. Hypertension. 2020 Oct;76:1045-1054.
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.

