Ketamine: Everyone's New Favorite Drug
Why is ketamine popping up everywhere? It is an old drug, but is it finally getting the spotlight after 50 years on the market?

This post will focus on use of ketamine in adult patients only (18 years or older).
Disclaimer: This post is meant to provide an overview of a clinical topic that may include (but is not limited to) information on pathophysiology, diagnosis, treatment, clinical pharmacology, medication management, adverse effects, and clinical pearls. References are included at the bottom of the post. This post is not to be used as medical advice for direct patient care, but as a guide for learning and discussion.

What is Ketamine?
Brand name: Ketalar
FDA approved: 19 February 1970
Drug Class: antidepressant; general anesthetic
Mechanism of action:
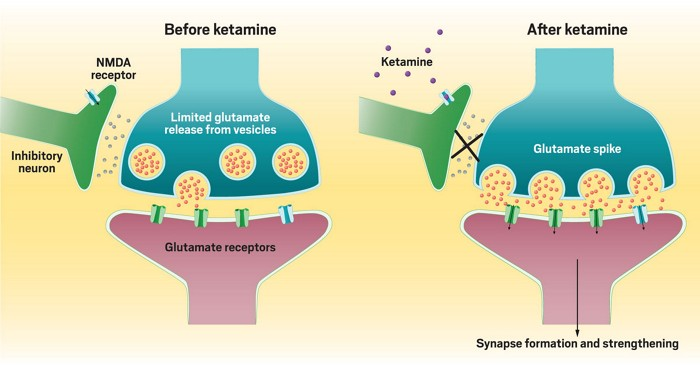
- Noncompetitive NMDA receptor antagonist that blocks glutamate (the excitement hormone/neurotransmitter) and increases glutamate release (see Figure 1 below).
- Directly acts on the cortex and limbic system to product a cataleptic-like state where the patient is dissociated from the surrounding environment.
- Low (subanesthetic) doses produce analgesia (the inability to feel pain) and modulate central sensitization, hyperalgesia and opioid tolerance. Lower doses also reduce polysynaptic spinal reflexes.
Brief Pharmacokinetics:
Half-life is 10-15 minutes for alpha, then 2.5 hours for beta
- Alpha stage is the initial slope in concentration lasting about 45 minutes. The first phase corresponds clinically to the anesthetic effect of the drug. The anesthetic action is terminated by a combination of redistribution from the CNS to slower equilibrating peripheral tissues and by hepatic biotransformation to metabolite I (norketamine). This metabolite is about 1/3 as active as ketamine in reducing halothane requirements of the rate.
- Beta stage refers to the later half-life of ketamine (2.5 hours)
Renally eliminated (so watch out for kidney function!)
Onset of action is seconds with IV, a few minutes for IM, and 10 minutes with intranasal. Oral onset is dose dependent but within 30 minutes
What is Ketamine used for?
Indications:
- Agitation (acute/severe/refractory)
- Analgesia, subanesthetic dosing
- Depressive episode associated with MDD
- General anesthesia
- Mechanically ventilated patients in the ICU, analgesia/sedation/agitation
- Procedural sedation
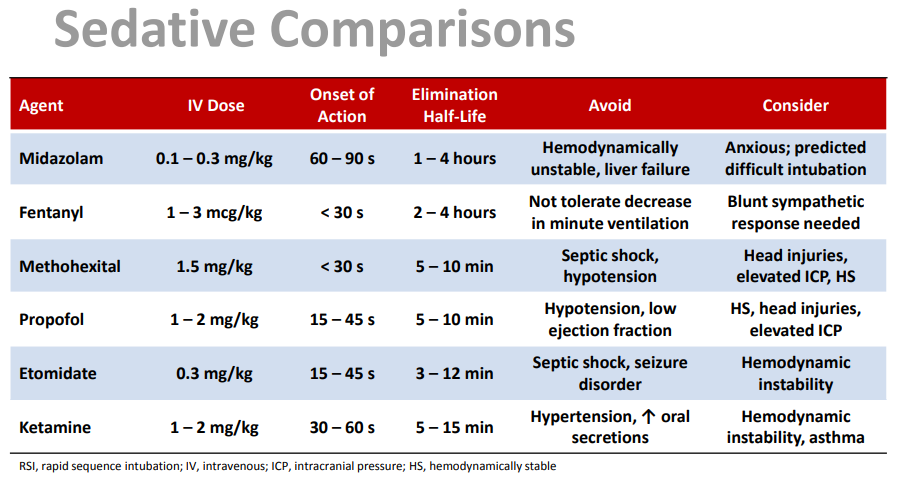
- RSI outside the operating room
- Status epilepticus, refractory
Dosing Ketamine
Weight based dosing using actual body weight and titrate to clinical effect
A general rule of thumb for bolus dosing that I use (especially when verifying orders in the Emergency Department):
0.01 mg/kg - 0.49 mg/kg = PAIN dosing
0.5 mg/kg - 2 mg/kg = ANALGESIC dosing
**IV bolus doses should be given over a period of 60 seconds; rapid administration can cause respiratory depression
Obesity recommendations (mainly for continuous infusions):
- BMI 30-39: use actual body weight
- BMI >40: use adjusted or ideal body weight
- Why? The volume of distribution (Vd) for ketamine is 2.1-3.1 L/kg (for reference vancomycin has a Vd of 0.7 kg/L). With such a large Vd, ketamine has a rapid peak anesthetic effect and a rapid loss of effect due to the redistribution into fat tissue in larger patients. Ketamine also has an active metabolite. Due to this, prolonged use may contribute to risk of accumulation and toxicity, especially in patients with BMI >40 due to accumulating in fat tissue.
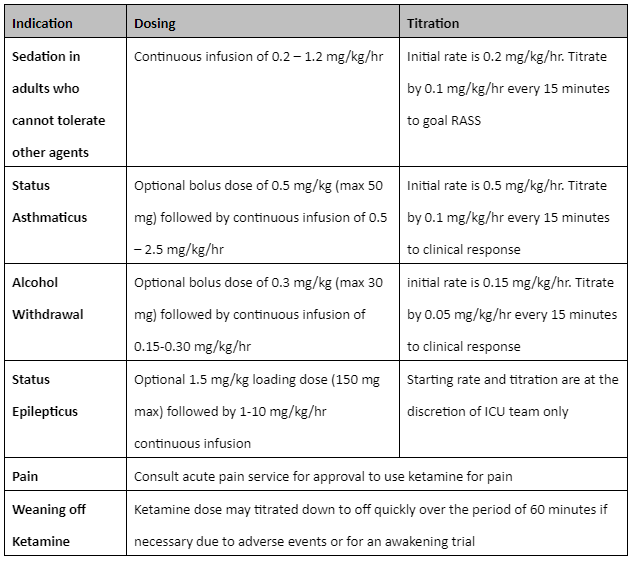
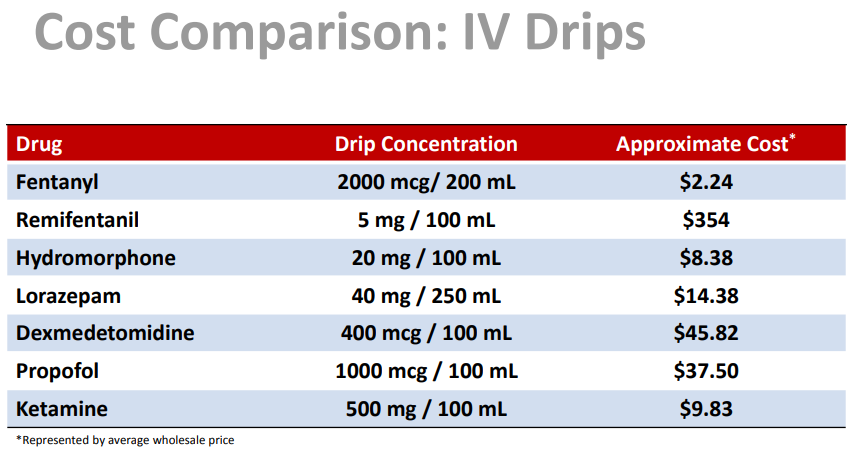
Recommendations from Michigan Medical Clinic (that I found useful for continuous infusions!)
Monitoring
- NOTE: Ketamine is known for emergence reactions, which can include agitative/combative episodes, and also emesis and laryngospasms.
- General: Pulse oximetry, vitals, and capnography
- Blood pressure: elevation of blood pressure shortly after injection. The SBP and DBP peak around 10-50% above preanesthetic levels
- Vision: Diplopia and nystagmus have been reported
- Respiratory status: if given by rapid bolus, can produce reductions in PaO2. Monitor supplemental oxygen while breathing room air
- Neuro: post-operative mental status
- Hormonal: can elevate plasma cortisol, renin, and prolactin
- Muscular: can increase skeletal muscle tone and produce muscle spasms

Why is Ketamine EVERYWHERE?
Benefits over other agents:
- Ketamine has a bronchodilatory effect. This is beneficial in asthmatic or COPD patients
- Ketamine has minimal net systemic vascular resistance change
- Ketamine increases cerebral metabolism and cerebral blood flow while producing a noncompetitive block of the glutaminergic postsynaptic NMDA receptor
- Ketamine exerts sympathomimetic effects by stimulating CNS outflow and decreasing catecholamine reuptake. This causes, in turn, a myocardial depressant action in stressed, catecholamine-deficient patients
- Ketamine is known to decrease serum free fatty acids
- Data suggests a profound analgesic effect and decrease in opioid consumption for up to six weeks

Caution use of Ketamine in patients with...
X = absolute contraindication
- X Patients with pre-existing history of schizophrenia or bipolar disorder
- Uncontrolled hypertension
- Pulmonary hypertension
- Moderate-severe hepatic dysfunction (Child-Pugh Class B and C)
- History of coronary artery disease
- Atrial arrhythmias
- Concomitant use of strong CYP3A4 and CYP2D6 inhibiting medications
- Preanesthetic elevated cerebrospinal fluid pressure
Clinical Application of Ketamine
- Ketamine is a good sedative option for patients with status asthmaticus.
- Other patients to use ketamine in: those that need pain control and aren't well controlled on fentanyl or other conventional sedation or opioid tolerant patients
- From my institution, we had a patient in the neuro critical care unit. This patient was on TPN, intubated, post-laparotomy with an ileus, and the providers would not give him opioids. Therefore, the patient was on massive doses of propofol, dexmedetomidine, and antipsychotics due to agitation (likely from uncontrolled pain). One of our pharmacists suggested ketamine for the patient. This was an excellent example for when to recommend ketamine!
Have a question about something above? Want to share your thoughts/advice with ketamine use? Comment below and start a conversation with us!
References:
- Lexicomp (2023). Lexi-Drugs. Wolters Kluwer. Updated June 27, 2023. Accessed May 2023. https://online.lexi.com.
- Michigan Medicine. Ketamine IV Continuous Infusion Guidelines for Mechanically Ventilated Adult ICU Patients. P&T reviewed 2020. https://www.med.umich.edu/surgery/mcccn/documents/Ketamine_Guideline_Adult_ICU.pdf
- White PF, Way WL, Trevor AJ. Ketamine—Its Pharmacology and Therapeutic Uses. Anesthesiology. 1982; 56:119–136. https://doi.org/10.1097/00000542-198202000-00007
- Tollings JL, Diedrich DA, Oyen LJ, et al. Rapid-Sequence Intubation: A Review of the Process and Considerations When Choosing Medications. Annals of Pharmacotherapy. 2014;48(1):62-76. doi:10.1177/1060028013510488
- White JM, Ryan CF. Pharmacological properties of ketamine. Drug and Alcohol Review. 1996; 15: 145-155. https://doi.org/10.1080/09595239600185801
- K Hirota, DG Lambert. Ketamine: new uses for an old drug? British Journal of Anaesthesia. 2011;107(2):123-126. https://doi.org/10.1093/bja/aer221
- Green SM, Roback MG, Kennedy RM, et al. Clinical Practice Guideline for Emergency Department Ketamine Dissociative Sedation: 2011 Update. Annals of Emergency Medicine. 2011;57(5):449-461. https://doi.org/10.1016/j.annemergmed.2010.11.030.

