The Danger of SALAD
First off, no, we are not talking about the leafy green, nutrient dense salads we eat every once in a while. SALAD is an acronym for "Sound Alike Look Alike Drugs." The Institute for Safe Medication Practices (ISMP) is an organization devoted entirely to preventing medication errors.

First off, no, we are not talking about the leafy green, nutrient dense salads we eat every once in a while. SALAD is an acronym for "Sound Alike Look Alike Drugs." Let's talk a little bit about the importance of this acronym and about a close call I encountered in the Burn Trauma Unit the other day.
The Institute for Safe Medication Practices (ISMP) is an organization devoted entirely to preventing medication errors.
At my hospital, we receive regular emails from our drug safety pharmacist about the ISMP newsletter. This weekly newsletter details updates, recent medication errors, education on potential mix ups, and other pertinent topics to medication safety across the country.
Regarding SALAD or "Look-alike and/or Sound-alike" medications (LASAs), these are medications that have similar generic names or similar packaging. Below are a few examples of look alike vials. Notice that the vial sizes and cap colors are nearly identical. If not read appropriately, or if barcode scanning is not used, the wrong vial of medication could be grabbed and administered to the patient.
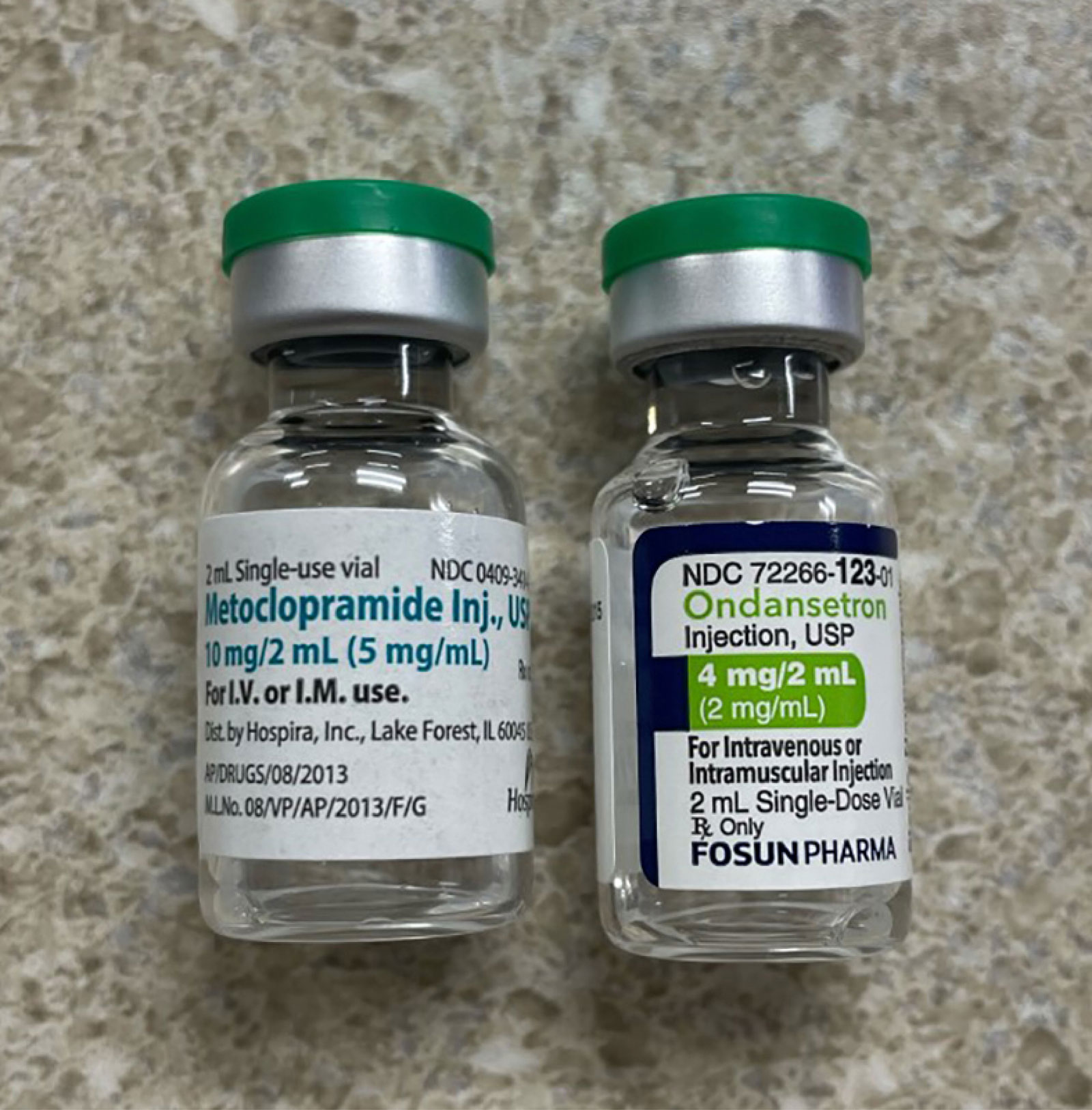
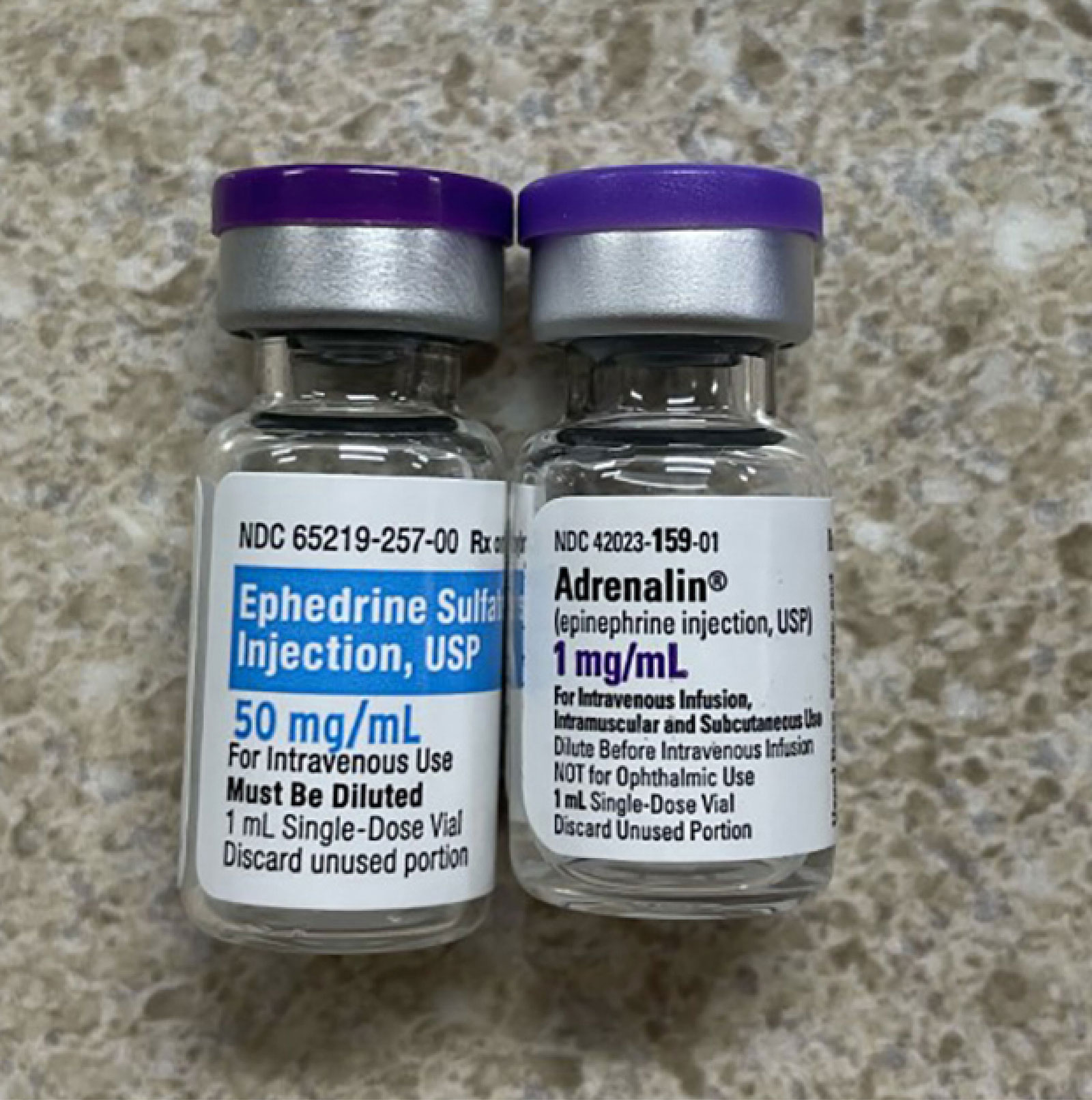
In the case of ephedrine and epinephrine in Figure 2, not only are the vials and cap colors similar, but the names of the medications are similar as well.
There are dozens of examples similar to the ones above. To mitigate errors, ISMP has developed resources to help educate practicing providers!
Use this list to determine which medications require special safeguards to reduce the risk of errors and minimize harm. This may include strategies such as:
1. Using both the brand and generic names on prescriptions and labels
2. Including the purpose of the medication on prescriptions
3. Configuring computer systems to require a minimum of the first five letters of a drug name during product searches
4. Changing the appearance of look-alike product names to draw attention to their differences
Both the FDA-approved and the ISMP-recommended Tall Man (mixed case) letters have been included in this list.
Tall Man Lettering
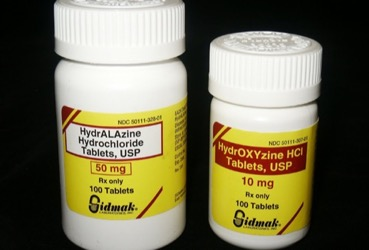
If you have ever stepped into a pharmacy, you likely noticed some drug names have capitalized and lowercased letters. This is a concept from ISMP called "Tall Man Lettering." There is a whole documented dedicated to this strategy for mitigating errors with sound-alike, look-alike medications.
Tall Man Lettering helps bring attention to SALAD. Below is a common example of hydrALAzine and hydrOXYzine.
For more information on how to implement precautions in your pharmacy, check out this guidance document from ISMP!
Clinical Scenario: Hydroxyurea or Urea?
Background: There was a patient admitted to the burn trauma unit (BTU) who had acute renal failure (ARF) and hyponatremia (sodium 126 on admission). The primary team taking care of the patient was the Trauma Team (makes sense). For ARF, nephrology was consulted. To correct the hyponatremia, the Trauma attending said on rounds to order "hydroxyurea." Doing as told, the resident ordered hydroxyurea. The order was verified by pharmacy, and the first dose was given the next morning.
My role: In the afternoon of the following day (so, after that first dose), I was working in central pharmacy. I answered a phone call from one of the nephrologists. The nephrologist wanted to know why a particular patient in the BTU was on hydroxyurea. I looked in the past medical history, but also did not see any clear indication for this medication. I was searching for problems such as sickle cell disease, leukemia, or some type of thrombocythemia or polycythemia. My search also included any recent diagnoses in the chart during this admission or a recent outpatient visit.
Continuing my discussion with the nephrologist, she told me the Trauma Team may have intended to order urea for the patient's hyponatremia. Upon further review of the patient's chart, I agreed. I told the nephrologist I would reach out to Trauma to correct this error.
Mechanism of Urea: normalizes serum sodium levels by inducing osmotic excretion of free water. Urea also ameliorates hyponatremia in syndrome of inappropriate antidiuretic hormone secretion by a more specific effect, diminishing the natriuresis in association with increased medullary urea content.
Source: Lexicomp 2023
I immediately tried to contact the Trauma Resident. When I asked why hydroxyurea was ordered (and if the team intended to order urea instead), he responded with "my attending said hydroxyurea during rounds so that is what I ordered."
Resident Learning Point: I further asked if he knew what that medication was for and if he questioned his attending. He said no. This is a note to all residents out there: the attending is not always right! Or, maybe you heard the attending incorrectly. Have a questioning attitude!
Pharmacist Learning Point: On the flip side, the verifying pharmacist also has a responsibility to the patient as legalized by the Tort Law and Omnibus Budget Reconciliation Act (OBRA 1990). The pharmacist should have looked into the patient's chart for an appropriate indication to start hydroxyurea therapy before verifying the order.
The Outcome: Regardless, the resident understood the mix up and allowed me to switch to an appropriate regimen of urea for the patient's hyponatremia. I went in and reported the error anonymously through my hospital's error reporting system, as the patient did receive a dose of inappropriate hydroxyurea. I followed up with the nephrologist who was thankful for my time on this issue. The patient's sodium corrected over the next few days, and they were discharged after resolution of all acute problems.
This is a great example of SALAD and the dangers of drug mix ups! Every member on the health care team is important. Always have a questioning attitude!