Parkinson’s vs. Parkinsonism: Pharmacotherapy
Accurate differentiation between Parkinson’s disease and other parkinsonian syndromes is key to guiding pharmacotherapy and optimizing patient outcomes.

Author: Madison Trombley, PharmD Candidate 2028
Editor: Kristen Lindauer, PharmD, BCPS, AAHIVP
Introduction
When a patient presents with tremor, rigidity, and bradykinesia, it is tempting to assume Parkinson’s Disease (PD). Although PD makes up a majority of parkinsonism cases, other, less prevalent conditions also fall under this umbrella. While these conditions share similar clinical features, pharmacotherapy can be challenging, as not all respond to the same treatments. Accurately distinguishing PD from other forms of parkinsonism is therefore essential to guiding appropriate therapy.
Parkinson’s Disease
PD is characterized by decreased dopamine levels, a result of degeneration of dopamine neurons in the substantia nigra. Diagnosis requires bradykinesia with one or both muscular rigidity and resting tremor. Additionally, the diagnosis of clinically established PD requires the absence of red flags. Diagnosing clinically probable PD allows for the presence of up to two red flags counterbalanced by supportive criteria. The presence of multiple red flags favors a diagnosis of atypical parkinsonism, which is covered in more detail below. Red flags and supportive criteria can be found in Table 1.
Levodopa is a first-line therapy for managing motor symptoms, as it crosses the blood-brain barrier and is converted to dopamine. It is commonly given in combination with carbidopa, which inhibits peripheral decarboxylation of levodopa, preventing premature breakdown in the plasma and increasing its availability in the brain.
MOA: Levodopa crosses the blood-brain barrier and is converted to dopamine.
Parkinsonism
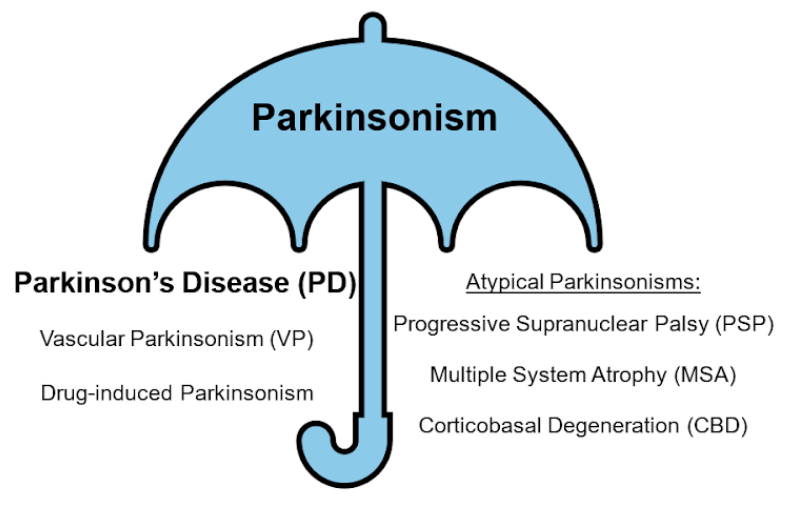
Parkinsonism is a neurologic syndrome characterized by tremor at rest, rigidity, bradykinesia, and postural instability. Parkinsonism itself is not a diagnosis, but rather a set of symptoms. Parkinsonism may be due to a variety of different causes, including (see Figure 1):
- PD
- Vascular parkinsonism (VP)
- Progressive supranuclear palsy (PSP)
- Multiple system atrophy (MSA)
- Corticobasal degeneration (CBD)
- Drug-induced parkinsonism
“Atypical parkinsonism” refers to a specific group of neurologic conditions that share several clinical features with PD, along with additional symptoms that progress faster and benefit less from medication. This group includes PSP, MSA, and CBD.
Table 1. Clinical signs and symptoms distinguishing PD from atypical parkinsonism

Pharmacotherapy
There are several different etiologies for parkinsonism, making pharmacotherapy challenging. Compared to PD, levodopa therapy is not always effective for patients presenting with other forms of parkinsonism, as shown in Table 2. In some instances, like PSP and MSA, patients may have an initial response to pharmacotherapy before refractory symptoms progress.
Currently, there is no treatment to slow or halt the progression of parkinsonism. Therefore, pharmacotherapy is used with palliative care to treat symptoms and improve quality of life.
Levodopa is a first-line therapy for managing motor symptoms.
Dopamine agonists, such as ropinirole or pramipexole, can be used as monotherapy before levodopa; they are less effective at improving motor symptoms, but are less likely to cause bradykinesia as an adverse event.
MAO-B inhibitors and COMT inhibitors are used in conjunction with levodopa/carbidopa and prolong the effects of levodopa.
Management of depression includes, but is not limited to, SSRIs. Monitor for side effects, including sedation and drowsiness.
Table 2. Levodopa effectiveness in each Parkinsonian condition.
Pharmacist’s Role
Managing parkinsonism requires not only careful selection of pharmacotherapy but also interdisciplinary collaboration, including neurology, speech therapy, physical therapy, and behavioral health. Pharmacists have various roles in managing parkinsonism.
Pharmacists can:
- Differentiate PD from parkinsonism
- Monitor levodopa efficacy
- Assess improvement in motor symptoms (tremor, rigidity, bradykinesia)
- Watch for “wearing off” between doses or delayed onset, suggesting underdosing or need for adjunct therapy
- Monitor blood pressure and mental status to balance efficacy with safety
- Screen for drug-drug interactions
- Dopamine receptor blockers
- Calcium channel blockers
- Antiarrhythmic drugs
- Lithium
- Optimize medication regimens
- Adjust levodopa timing and formulation to improve motor control
- Recommend dosage increase or adjunct therapy when “wearing off” occurs
- Suggest dose reductions or discontinuation of offending agents in drug-induced parkinsonism
- Educate patients and caregivers
- Counsel on proper administration
- Set realistic expectations about symptom relief and long-term progression
- Encourage adherence and monitoring for safety and efficacy
About the Author

References
- Shrimanker I, Tadi P, Schoo C, et al. Parkinsonism. [Updated 2024 Mar 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542224/
- Parkinson Disease – DynaMed. 2025. https://www.dynamed.com/condition/parkinson-disease#GUID-23DF2968-E4FB-4E87-AFA2-140CAC157BA9
- Koch, Jessa M., et al. "Parkinson Disease." DiPiro’s Pharmacotherapy: A Pathophysiologic Approach, 12th Edition Eds. Joseph T. DiPiro, et al. McGraw Hill, 2023, https://accesspharmacy.mhmedical.com/content.aspx?bookid=3097§ionid=265902106.
- Carbidopa and Levodopa (Lexi-Drugs) - UpToDate® LexidrugTM. 2025. https://online-lexi-com.eu1.proxy.openathens.net/lco/action/doc/retrieve/docid/patch_f/7167?cesid=4JhYjLA8zSK&searchUrl=%2Flco%2Faction%2Fsearch%3Fq%3Dlevodopa%26t%3Dname%26acs%3Dfalse%26acq%3Dlevodopa
*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.

