Potassium and Hypertension
Increasing potassium intake lowers blood pressure, reduces stroke risk, and may decrease antihypertensive medication needs.

Hypertension is the leading cause of cardiovascular morbidity and mortality worldwide. It damages blood vessels by causing inflammation, scarring, plaque buildup, and more. It does this silently in the background of everyday life, oftentimes with no noticeable symptoms for years. The good news is that it is a modifiable risk factor. The new 2025 ACC/AHA Hypertension Guidelines place greater emphasis on lifestyle modifications as a foundation for blood pressure control and dietary changes are a cornerstone of this approach.
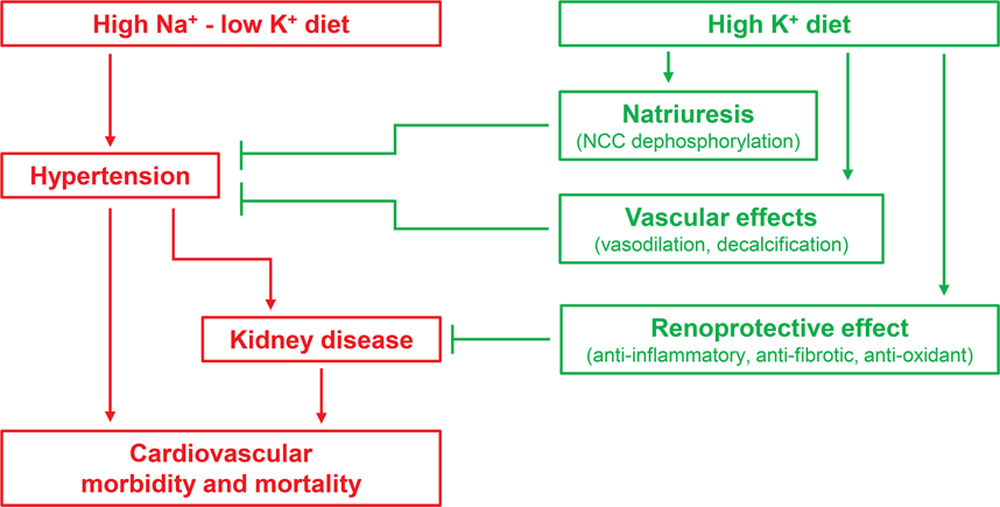
While decreasing sodium intake gets most of the spotlight in this area, increasing potassium intake is an important yet sometimes overlooked strategy. Potassium and sodium go hand in hand, with increased potassium resulting in decreased sodium retention in the body. While cutting sodium in the diet can be difficult in practice, increasing potassium may be a more approachable way to decrease the amount of sodium retained in the body and counteract sodium’s harmful impact on blood pressure.
How Does It Work?
Potassium lowers blood pressure primarily through two mechanisms:
- Vasodilation: More potassium in the blood hyperpolarizes the endothelial cell via stimulation of the sodium pump and opening of potassium channels, resulting in relaxation of the blood vessels and a decrease in peripheral resistance.
- Natriuresis: A high potassium diet promotes downregulation of the sodium chloride cotransporter, leading to sodium excretion and reduced blood volume.
What Does the Data Say?
- Lower BP: A meta-analysis from the World Health Organization, including 22 randomized controlled trials, reported that increased potassium intake lowered systolic blood pressure by 5.3 mmHg and diastolic blood pressure by 3.1 mmHg in individuals with hypertension. A potassium intake in line with ACC/AHA recommendations of 90-120 mmol/day resulted in a systolic blood pressure decrease of 7.2 mmHg.
- Stroke Reduction: The same meta-analysis showed risk of stroke decreased by 24%. A separate 12-year prospective study showed that a potassium increase of 10 mmol/day resulted in a 40% reduction in stroke mortality.
- Less Medication: A randomized controlled trial showed that 81% of participants needed less than half of their baseline antihypertensive medication, and 29% needed no medication to achieve adequate blood pressure control, versus 29% and 9% in the control group, respectively.
- Reduced Hypertensive Risk: A cluster randomized controlled trial showed that patients who used a salt substitute of 75% sodium chloride and 25% potassium chloride had a 51% reduced risk of developing hypertension compared to controls. Notably, the use of the salt substitute also decreased sodium consumption by 8% and increased potassium consumption by 57%.

How to Increase Potassium Consumption
The ACC/AHA Hypertension Guidelines recommend a potassium intake of 3,500-5,000 mg per day. Average potassium intake in North America is only 2,500-2,700 mg per day, well below recommendations. The AHA encourages meeting potassium needs primarily through food rather than supplementation. Potassium can be found naturally in a variety of foods:
- Fruits: bananas, oranges, apricots, cantaloupe
- Vegetables: spinach, potatoes, tomatoes, broccoli, yam
- Dairy products: milk, yogurt
- Legumes: beans, lentils
Additionally, potassium-based salt substitutes (like Morton Lite Salt) are an effective way to introduce potassium into the diet while also reducing sodium intake without significant dietary modification.
Safety Considerations
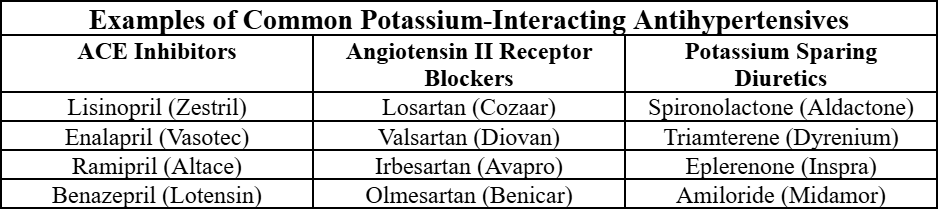
Although dietary potassium is generally safe, it is important to note that not all patients should increase their intake freely without consulting a medical professional. Patients with impaired renal function or those taking ACE inhibitors, ARBs, or potassium-sparing diuretics are at an increased risk of hyperkalemia. Symptoms of hyperkalemia include nausea, vomiting, irregular heart rate, fainting, and muscle weakness.
Conclusion
The increased emphasis on lifestyle modifications for both treatment and prevention in the latest hypertension guidelines makes knowledge about dietary changes for blood pressure control even more relevant. For pharmacists and pharmacy students, the ability to counsel patients on potassium intake, recognize who stands to benefit most, and know when to exercise caution will be essential. Although hypertension remains a leading global health challenge, something as simple as increasing potassium intake can make a measurable difference in patient outcomes.
References:
- Aburto, N. J., Hanson, S., Gutierrez, H., Hooper, L., Elliott, P., & Cappuccio, F. P. (2013). Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ, 346(apr03 3), f1378–f1378. https://doi.org/10.1136/bmj.f1378
- American Heart Association. (2015). How Potassium Can Help Control High Blood Pressure. Heart.org. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/how-potassium-can-help-control-high-blood-pressure
- Chan, R., Parikh, N., Ahmed, S., Ruzicka, M., & Hiremath, S. (2023). Blood Pressure Control Should Focus on More Potassium: Controversies in Hypertension. Hypertension, 81(3). https://doi.org/10.1161/hypertensionaha.123.20545
- Khaw, K.-T., & Barrett-Connor, E. (1987). Dietary Potassium and Stroke-Associated Mortality. New England Journal of Medicine, 316(5), 235–240. https://doi.org/10.1056/nejm198701293160502
- Neal, B., Wu, Y., Feng, X., Zhang, R., Zhang, Y., Shi, J., Zhang, J., Tian, M., Huang, L., Li, Z., Yu, Y., Zhao, Y., Zhou, B., Sun, J., Liu, Y., Yin, X., Hao, Z., Yu, J., Li, K.-C., & Zhang, X. (2021). Effect of Salt Substitution on Cardiovascular Events and Death. New England Journal of Medicine, 385(12). https://doi.org/10.1056/nejmoa2105675
- Siani, A. (1991). Increasing the Dietary Potassium Intake Reduces the Need for Antihypertensive Medication. Annals of Internal Medicine, 115(10), 753. https://doi.org/10.7326/0003-4819-115-10-753