Updates in Heart Failure
What is new in the heart failure world when it comes to pharmacotherapy? Dr. Kiley is here to talk all about the new trials and drug approvals with us today!

Author: Patrick Kiley, PharmD
Editor: Kristen Lindauer, PharmD, BCPS
We have a special edition for you this week! Dr. Patrick Kiley, a current PGY1 resident at Sentara Norfolk General Hospital, recently presented a continuing education to our health system. He spoke about updates in heart failure therapy. Today, we will provide an overview of his objectives and talk a little about each one.
Dr. Kiley’s full PowerPoint presentation will be available to paid subscribers only. His PowerPoint contains his slide notes, educational graphics, and references! To access, click on the “Subscribe” button on the homepage and selected the tier you would like to subscribe to for premium RxTeach content!
Let’s get into the topic!
Dr. Kiley covered 6 objectives in his 60-minute presentation. You can find them below!
OBJECTIVE 1: Understand the etiology and pathophysiology of heart failure
What causes heart failure? As you may have guessed, other heart diseases can ultimately lead to the development of heart failure such as:
- Myocardial infarction (heart attack)
- Coronary artery disease
- Valvular disease
- Myocarditis (inflammation of the heart muscle)
- Arrhythmias (atrial fibrillation, atrial flutter, etc.)
- Diabetes (okay, not a heart disease, but can still lead to heart failure!)
- Congenital heart disease
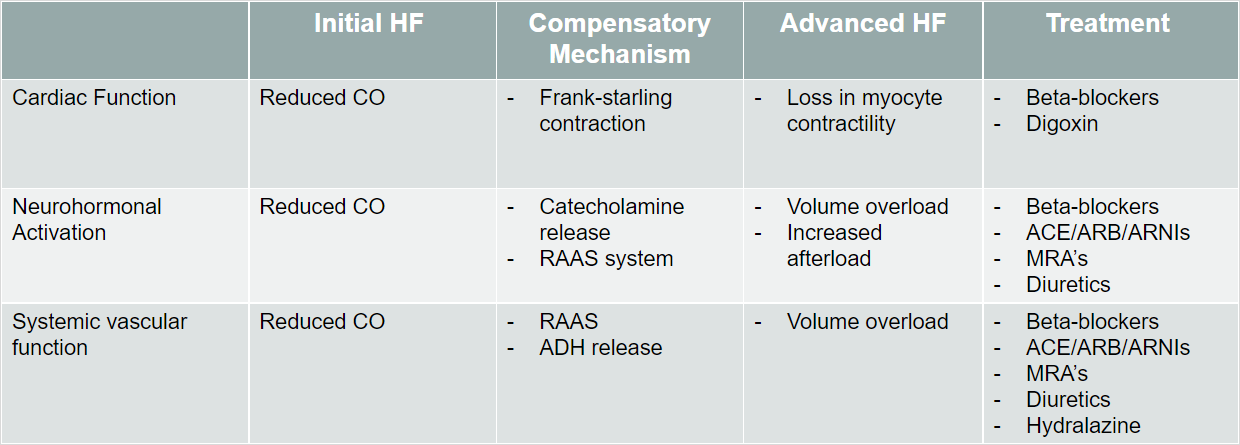
The pathophysiology (or, how a disease develops) for heart failure is multifactorial.
OBJECTIVE 2: Discuss previous and updated classifications of heart failure
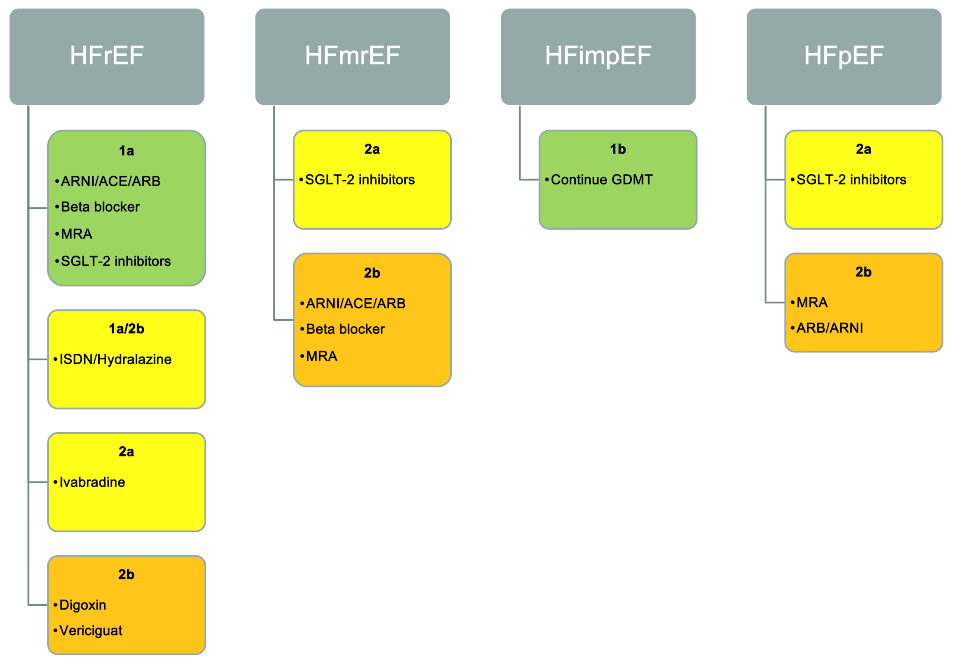
Prior to the 2022 guideline update, there was Heart Failure with Reduced Ejection Fraction (HFrEF) and Heart Failure with Preserved Ejection Fraction (HFpEF). Now, there are 2 more classifications of heart failure!
The additional classifications, Heart Failure with Mildly Reduced Ejection Fraction (HFmrEF) and Heart Failure with Improved Ejection Fraction (HFimpEF), allow for a better understanding and continuum of care for patients.
For example, if a patient has a baseline LVEF ≤40%, but then has a ≥10-point increase from baseline LVEF after being on guidelines directed medical therapy (GDMT), and this new measurement is >40%, they are now classified as HFimpEF and NOT HFrEF. this allows healthcare professionals to understand that GDMT is working for the patient, and they are improving!
In addition, the HFmrEF category is emerging in the literature. Many studies show morbidity and mortality benefits in patients with an EF <40% and in subgroups when the EF is <50%. Prior to the 2022 update, there was no good way to keep track of patients who had an EF between 40-50%, as they were all lumped under HFpEF. With the new HFmrEF category, providers are more aware of what GDMT the patient will best benefit from!

OBJECTIVE 3: Review symptom management and diuretic strategies
Diuretics have no data for mortality benefit, but they do help with symptomatic disease. Heart failure symptoms are typically from a build up of fluid. Often, patients will be asked to monitor their weight. If the patient notices an abnormal increase in weight, they are likely fluid overloaded. They will also notice it is more difficult to breathe with minimal activity.
One of the strategies to control these types of symptoms is prescribing diuretics. There are loop diuretics and thiazides/thiazide-like diuretics. Thiazide diuretics may be added to loop diuretics in refractory edema unresponsive to loop diuretics.
- Loop diuretics (furosemide, bumetanide, torsemide) inhibit reabsorption of sodium at the ascending Loop of Henle
- Thiazide/thiazide-like diuretics (chlorthalidone, metolazone, hydrochlorothiazide) inhibit compensatory distal tubular sodium reabsorption
A propensity analysis comparing high-dose loop diuretics vs. adjuvant metolazone found the addition of metolazone led to:
- Hypokalemia
- Hyponatremia
- Worsening renal function
Takeaway: Up titration of loop diuretics may be preferred vs. early initiation of thiazide diuretics
New information was published in 2022 about the use of Acetazolamide in Acute Decompensated Heart Failure with Volume Overload (ADVOR). A breakdown of the ADVOR trial can be found in Dr. Kiley's full presentation.
OBJECTIVE 4: Summarize guideline therapy recommendations for each classification
*This will be a tl;dr version. For more information, become a paid subscriber for access to the full PowerPoint below!

OBJECTIVE 5: Present updated iron recommendations in anemia
Iron deficiency:
- Ferritin <100mcg/L or 100-300 if Tsat <20%
Anemia in patients with HF is associated with impaired erythropoietin production. However, a randomized controlled trial of darbepoetin alpha in 2278 patients showed no benefit and increased thrombotic events. A Meta-analysis of 13 trials supported these findings. Therefore, Therefore, therapy with erythropoietin stimulating agents (ESAs) is not recommended for treatment of anemia in HF.
Oral iron has shown to be ineffective in clinical trials for patients with HFrEF (IRONOUT HF study is one example). It is recommended to supplement with IV iron. For example, weekly IV ferric carboxymaltose improved NYHA classification and quality of life in the FAIR-HF study.
The AFFIRM-AHF trial published in 2020 was the first trial to show a reduction in HF hospitalization after supplementation with IV iron compared to placebo in patients with LVEF <50%. No reduction in CV death was found. There are trials currently underway aiming to show a mortality benefit with IV iron in our HF population (FAIR-HF-2 study).
As for patients with HFpEF, literature around the benefits of iron therapy is less clear (one meta analysis from Beale AL, et al. 2019 on this topic). There may be some benefit. It is appropriate to trial oral iron supplementation in HFpEF patients until more data proves otherwise.
OBJECTIVE 6: Recognize newer agents recommended in heart failure
For this section, we are going to focus on vericiguat. This is the most recent medication added the HF guidelines.
Vericiguat is for high risk patients with HFrEF and recent worsening of HF on GDMT. Vericiguat may reduce HF hospitalizations and CV death.
Mechanism of action: oral soluble guanlyate cyclase stimulator that directly binds and stimulates sGC increasing cGMP. This results in vasodilation, improvement in endothelial function, and decrease in fibrosis and remodeling of the heart.
This medication should be avoided in pregnancy and can cause orthostatic hypotension in the general population. Vericiguat has significant drug-drug interactions with phosphodiesterase 5 inhibitors and riociguat.
Dr. Kiley covers more on vericiguat from the VICTORIA trial in his full PowerPoint.
Thank you, Dr. Kiley, for a great update on heart failure treatment! We are excited for what the future holds for you and your career after residency!