Exercise Extends Life After Cancer Diagnosis
New data published in NEJM last month showcases additional benefits of exercise not previously well described; extending survival in cancer patients.

Over the years, RxTeach has produced countless articles on the benefits of exercise in preventing diseases like diabetes, cardiovascular disease, and even cancer. We've known for a long time that regular exercise increases both health-span and life-span while simultaneously enhancing quality of life. However, new data published in NEJM last month showcases additional benefits of exercise not previously well described; extending survival in cancer patients.
This is the first time we've seen strong randomized Phase 3 data supporting exercise as an intervention in cancer patients. Courneya et al. published their findings from a randomized trial conducted at 55 centers across Canada, Australia, France, the United States, and the UK. Patients with resected colon cancer who had completed adjuvant chemotherapy were randomized to participate in a structured exercise program (exercise group) or to receive health-education materials alone (health-education group) over a 3-year period. The primary end point was disease-free survival (DFS).
For those unfamiliar with oncology endpoints, DFS measures the amount of time from tumor removal to either death or disease recurrence. These patients all received adjuvant chemotherapy, which means they received chemo after their tumor was removed. In this case, patients were randomized 2-6 months after chemotherapy, so any patients that were unable to tolerate chemo were excluded.
The study randomized a total of 889 patients with a median follow-up of 7.9 years. The results are incredible. HR for DFS was 0.72; 95% confidence interval [CI], 0.55 to 0.94; P=0.02). This means that exercise reduced patients' risk of dying or having their cancer come back by 28%.
When looking strictly at survival, hazard ratio for death was 0.63; 95% CI, 0.43 to 0.94), meaning that exercise reduced patients' risk of dying by 37%. The absolute OS risk reduction was 7% at 8 years. Let's compare that to other oncologic agents used after surgery across different tumor types.
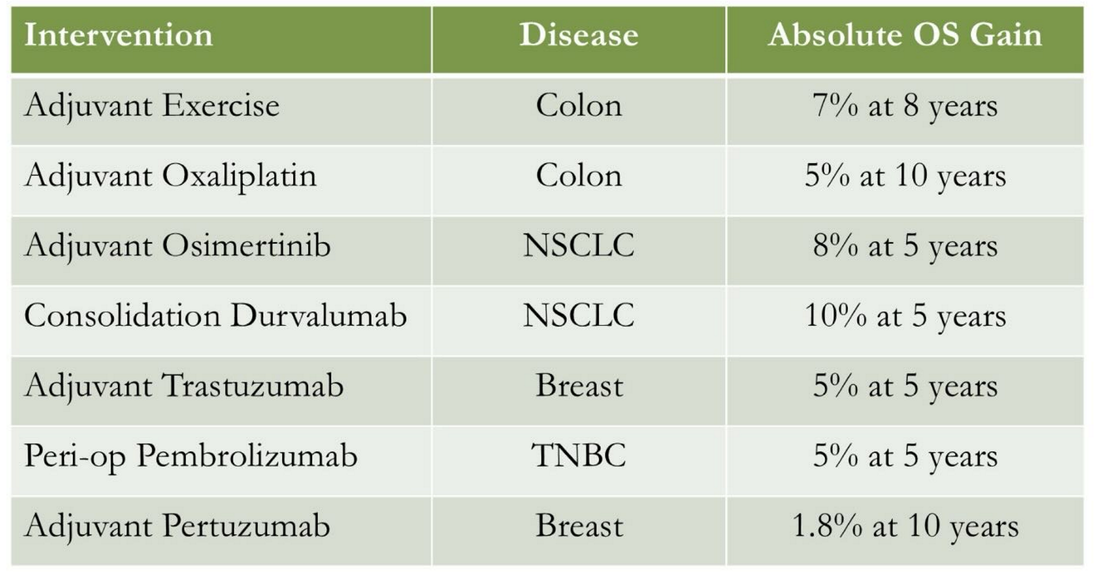
As you can see, exercise is just as effective as many of these other more toxic and expensive interventions! Unlike oncologic agents, which typically come with a long list of adverse events, exercise is totally benign. There were essentially zero differences in safety outcomes between groups in this study. The exception is musculoskeletal adverse events (pulled muscles, sprained ankles, etc..) which occurred in 18.5% vs. 11.5% of patients in the exercise and non-exercise groups respectively. Importantly, only 10% of the musculoskeletal adverse events were considered related to the exercise intervention. Speaking for myself, I would undoubtedly accept a 7% absolute risk increase of mild injury in return for a 37% relative risk reduction of death. NOTE: This does not mean cancer patients should stop taking their medications and do exercise instead. They should of course be doing both, as recommended under the advisement of their treating physician.

This data supports findings from previous observational studies and retrospective meta-analysis. With that history, these results aren't exactly surprising, and most people inherently understand that exercise is good for you. Still, it is so cool to finally have prospective randomized data in cancer patients for an intervention that costs them nothing.
According to the authors, the exercise group experienced "improved overall survival, patient-reported physical functioning, and objective physical functioning and fitness as compared with health education alone, with only a modest increase in musculoskeletal adverse events." I'm thrilled to have access to this data, and I commend the authors for doing this important work. You can check out some of our prior posts on exercise below.






*Information presented on RxTeach does not represent the opinion of any specific company, organization, or team other than the authors themselves. No patient-provider relationship is created.